1. Introduction
Fibrotic diseases are common and can affect almost all organs, accounting for approximately 40% of deaths in Western countries. Although the initial triggers vary—ranging from toxins and infections to radiation and other factors —tissue injury ultimately leads to a chronic inflammatory process. Depending on the type of injury and an individual’s genetic or epigenetic background, the activation of mesenchymal cells results in excessive deposition of extracellular matrix (ECM) in the affected tissues [
1,
2,
3,
4].
Despite distinct etiological and clinical features, most chronic fibrotic disorders share common characteristics, including the recruitment of inflammatory cells and sustained production of growth factors, angiogenic factors, and fibrogenic cytokines. These factors activate effector cells, leading to the excessive deposition of ECM by myofibroblasts, pericytes, and other fibroblast subsets [
3,
5]. While early fibrotic responses may be reversible through enzymatic degradation of ECM components, pathological tissue remodeling—such as in liver cirrhosis, cardiovascular fibrosis, localized and systemic scleroderma, chronic kidney disease, and idiopathic pulmonary fibrosis—is considered irreversible after a certain stage, potentially progressing to organ failure and death [
6].
Therapeutic intervention in fibrotic processes has proven challenging. Numerous attempts have been made to modulate the immune system, interfere with specific cytokine activity, inhibit ECM crosslinking, or eliminate activated mesenchymal cells. However, targeting the synthesis and secretion of ECM molecules remains difficult due to the risk of severe side effects associated with pharmacological interventions. In recent years, significant progress has been made in understanding the complex secretion of large molecules via the endoplasmic reticulum (ER). Here, we discuss various approaches to directly interfere with collagen secretion, the primary structural component of the ECM, as a potential antifibrotic strategy.
2. The Extracellular Matrix
The ECM is composed of a wide variety of components, including collagens and numerous glycoproteins such as fibronectin, fibrillins, elastin, fibulins, tenascins, thrombospondins, and various proteoglycans [
7,
8]. Collectively, these components form the ECM, which, with associated proteins, is also referred to as the “matrisome” [
9,
10,
11]. The composition and interactions of these molecules determine the structure of extracellular networks [
7,
12], which, in combination with cellular constituents, regulate the biomechanical properties, rigidity, and stiffness of connective tissues [
11,
13,
14]. Alongside collagens, these ECM molecules are embedded in amorphous structures containing glycoproteins (e.g., fibronectin), proteoglycans, and hyaluronan, all of which contribute to the biomechanical properties of the ECM [
7,
15]. The ECM provides structural and biomechanical support to cells, guiding migration by serving as a scaffold and presenting signalling cues, while also influencing proliferation, differentiation, and transdifferentiation through mechanochemical signaling and growth factor regulation. By modulating cell-ECM interactions, the ECM can induce phenotypic changes, promote tissue-specific differentiation, or even facilitate transdifferentiation by altering transcriptional programs in response to dynamic microenvironmental cues [
11].
Interstitial fibrillar collagens are the primary structural components of connective tissues. All collagen molecules consist of three α-chains, characterized by a repeating Gly–X–Y sequence, where glycine occurs at every third position, and proline (X) and hydroxyproline (Y) contribute to the formation of the triple-helical structure unique to collagens. The collagen family comprises 28 proteins that form diverse structures and can be divided into classes ().
.
The collagen family.
| Collagen Classes and Their Macromolecular Organization |
Collagen Types [16] |
| Fiber forming collagens |
Collagens I, II, III, V, XI, XXIV |
| Network forming collagens |
Collagens IV, VIII, X |
| Beaded filaments forming collagens |
Collagen VI |
| Anchoring fibrils forming collagens |
Collagen VII |
| Fibril associated collagens with interrupted helices (FACIT) |
Collagens IX, XII, XIV, XIX, XX, XXI, XXII |
| Transmembrane collagens |
Collagens XIII, XVII, XXIII, XXV |
| Multiplexins |
Collagens XV, XVIII |
In skin and other loose connective tissues, classic fibrils visualized by electron microscopy contain mixtures of collagens I, III, V, XII, and XIV [
12]. Collagen VI, by contrast, exhibits a unique macromolecular organization within the microfibrillar network, characterized by a typical beaded filament appearance. Type IV collagen is a major structural component of basement membranes, while types VII and XVII anchor basement membranes to the underlying mesenchymal tissue [
10,
17]. Many of these collagens are synthesized by fibroblasts within connective tissues.
In fibrotic tissues, the ECM becomes excessively dense due to the abnormal deposition and arrangement of its components, along with aberrant crosslinking. This leads to increased tissue stiffness, contractures, and functional impairment [
2,
3,
5,
14,
18]. The biomechanical characteristics of the ECM are largely determined by interactions between elastin and the microfibrillar network. Elastin, which contains numerous crosslinks [
19], can adapt structurally to biomechanical demands. Elastin interacts with various microfibrillar components, including fibrillins, fibulins, matrilins, tenascins, and EMILINs, as well as latent TGF-β binding proteins (LTBPs) [
20,
21,
22,
23,
24,
25]. ECM components interact with cells at multiple levels. Fibroblasts, for instance, bind to ECM components via specific integrin receptors—heterodimeric transmembrane proteins that recognize distinct motifs within ECM molecules. These receptors not only mediate cell adhesion but also transmit mechanical forces and activate intracellular signaling pathways.
Four integrins have been identified that specifically bind collagen, each associated with distinct cellular functions [
26,
27,
28]. In addition to integrins, fibroblasts express collagen-binding receptors from the discoidin domain receptor (DDR) family, as well as other mechanosensitive receptors capable of detecting extracellular mechanical stress [
29,
30]. The role of biomechanical forces in cellular differentiation and function is a rapidly expanding field with significant implications for fibrosis pathophysiology [
15,
31].
Furthermore, proteolytic fragments derived from ECM cleavage, known as matrikines [
32,
33] or matricryptins [
34], exert various biological effects on inflammatory cells and fibroblasts. These fragments, generated from collagen, elastin, laminins, and proteoglycans, influence cell behavior and contribute to fibrotic processes [
35,
36]. Of note, proteolytically cleaved fragments can exert activities that differ considerably from those of the uncleaved parental ECM component [
34]. Finally, the ECM serves as a reservoir for cytokines and growth factors, regulating their bioavailability through controlled binding and release. This role has been particularly well documented for transforming growth factor-beta (TGF-β), which is synthesized as an inactive precursor bound to latent TGF-β binding proteins (LTBPs) [
37]. LTBPs, in turn, interact with fibrillins (fibrillin-1 and -2) that are key structural components of the microfibrillar system [
38,
39,
40,
41]. Mutations in fibrillin-1 or its associated binding partners lead to excessive fibrotic responses, as observed in congenital disorders characterized by stiff fibrotic skin, such as stiff skin syndrome (SSkS, OMIM: #184900) [
42,
43]. Fibrillin-dependent mechanisms of fibrosis have been modeled in the tight skin mouse (Tsk), which has been instrumental in advancing therapeutic strategies for fibrosis [
43]. The regulated release of TGF-β and other signaling molecules from the ECM underscores its dynamic role in the initiation and progression of fibrosis [
31,
44,
45,
46,
47].
Collagen biosynthesis is a highly complex process. Triple-helical collagens are synthesized as precursor molecules known as procollagens, which undergo extensive post-translational modifications, including hydroxylation of proline and lysine residues. After assembly into triple-helical structures, these collagens are exported from the ER. However, the precise mechanisms regulating their transport along the secretory pathway have only recently begun to be elucidated [
48,
49,
50,
51,
52,
53,
54].
In the extracellular space, procollagen propeptides at both termini are cleaved to allow the aggregation of collagen molecules into fibrils. These fibrils are subsequently crosslinked to form insoluble structures that provide tensile strength and stability to tissues [
55]. Given the complexity of collagen biosynthesis, multiple points exist for potential therapeutic intervention. Strategies have been explored to:
- -
-
Modulate cytokine-receptor signaling that induces collagen gene expression.
- -
-
Influence the formation of the triple-helical structure, which depends on the hydroxyproline content, or
- -
-
Inhibit lysyl oxidase, the enzyme responsible for stabilizing collagen crosslinks.
Until recently, less attention has been given to directly controlling the secretion of collagen or other large ECM molecules, which could represent a novel approach to antifibrotic therapy. In addition, several therapeutic approaches have been initiated more recently to modulate the cellular activation responsible for the synthesis of ECM proteins (
); however, the success of most interventions has remained disappointing.
.
Therapeutic Strategies to Inhibit Collagen Deposition in Fibrosis.
| 1 |
Inhibition of cytokine/growth factor signaling by monoclonal antibodies, small ligand inhibitors or blockade of intracellular signaling pathways |
[56] |
| 2 |
Inhibition of integrin signaling (αvβ6, α11β1) |
[29,57] |
| 3 |
Modulation of fibroblast and tissue stiffness |
[58,59] |
| 4 |
Inhibition of collagen prolyl hydroxylase |
[60,61] |
| 5 |
Inhibition of lysyl oxidase (LOX) and LOX-like enzymes (LOXL) 1–4 |
[62,63] |
| 6 |
Modulation of collagenolytic enzymes, targeting matrix metalloproteinases |
[64] |
| 7 |
Regulating the metabolic control of collagen synthesis |
[65] |
| 8 |
Modulation and ablation of activated fibroblast subsets |
[66,67] |
3. TANGO1 Builds a Secretory Route for Collagens
The ER is the gateway to the secretory pathway, where proteins are synthesized, folded, and assembled. Nearly a third of the proteome passes through the ER, underscoring its central role in cellular homeostasis. Secretory cargo, including large molecules like collagen, must be properly folded by molecular ensembles of ER chaperones [
68] before export to the ER-Golgi Intermediate Compartment (ERGIC) or Golgi apparatus.
ER export is mediated by Coat Protein Complex II (COPII) coat machinery, which assembles at specialized subdomains called ER exit sites (ERES). At these sites, COPII-dependent carriers package secretory cargoes for their transport to the next secretory compartment. COPII-dependent vesicles form when the ER-localized GEF Sec12 activates Sar1, a cytosolic GTPase, which then inserts into the ER bilayer and initiates coat assembly. Sar1 recruits an inner COPII layer of Sec23/24, which selects cargo, while an outer layer formed by a heterotetramer of Sec13/31 forms a polyhedral structure to mould the membrane and drive the budding of a vesicle with a diameter of 60–80 nm [
69]. However, these conventional COPII vesicles are too small to accommodate bulky cargo like collagen, necessitating adaptations at ERES in metazoan cells for ECM protein transport—the basis of metazoan multicellularity and 70% of our dry body weight.
To meet the challenge of exporting bulky secretory cargoes, animals have evolved TANGO1—a transmembrane protein localized at ERES in all animal species, essential for the secretion of large proteins [
70]. TANGO1 was discovered through a genome-wide RNAi screen in Drosophila S2 cells that identified genes required for the secretion of a generic secretory protein, signal-sequence containing horseradish peroxidase (ss-HRP) [
71]. Any ‘hit’ in the screen was a gene that affected protein Transport ANd Golgi Organization (TANGO). Several TANGO genes have been studied, renamed, a previously uncharacterized gene stood out, which was named TANGO1 [
72].
TANGO1 belongs to the Melanoma Inhibitory Activity (MIA) gene family. In invertebrates, this family is represented solely by MIA3, which encodes TANGO1. In vertebrates, gene duplication produced MIA2 and MIA3; MIA2 encodes TANGO1-like (TALI) and Cutaneous T-cell lymphoma-associated antigen 5 (cTAGE5), while MIA3 encodes long and short isoforms of TANGO1 [
70,
73].
At ERES, TANGO1 assembles into a ring-like structure and functions through distinct domains (). Its luminal SH3-like domain binds to collagen or Heat Shock Protein 47 (HSP47), ensuring that only properly folded, triple helical collagen is exported from the ER. Within the membrane, TANGO1 transmembrane helix and a membrane-inserted helix form a local diffusion barrier that isolates ERES from the rest of the ER. Finally, in the cytoplasm, TANGO1 binds to COPII components (Sec16, Sec23) via a C-terminal proline rich domain (PRD), to cTAGE5 via a coiled coil domain (CC2; see ), and the Neuroblastoma-amplified-sequence—Rad50-interacting protein 1—Zeste White 10 (NRZ) retrograde multisubunit tethering complex via another coiled-coil domain (CC1; see ), thereby coordinating cargo selection and membrane remodeling [
51,
74,
75,
76,
77,
78]. By recruiting ERGIC membranes, TANGO1 can generate and stabilize transient tunnels between the ER and ERGIC, bypassing vesicle formation altogether and allowing cargo export without size or shape constraints [
50,
70].
Thanks to these properties, TANGO1 is essential for collagen secretion, and its loss disrupts development across species [
79,
80,
81,
82,
83,
84]. In animal models—including fruit fly, zebrafish, mice, and dogs—loss or truncation of TANGO1 impairs collagen export and causes skeletal defects. In humans, mutations in the MIA3 gene, which encodes TANGO1, are linked to Ehlers–Danlos-like syndromes, dental and skeletal abnormalities, and in severe cases, prenatal lethality along with failed bone formation. Some individuals with truncated TANGO1 also show mild intellectual disability, suggesting a broader role for TANGO1 in the secretion of ECM and brain-enriched glycoproteins essential for development [
80,
82,
85]. The paralogue of TANGO1—TALI, performs a similar role in the ER export of bulky lipoproteins such as chylomicrons and vLDLs [
86,
87].
. TANGO1 reorganizes ER exit site machinery to build an ER–ERGIC tunnel. (<b>A</b>) COPII vesicle budding begins when the small GTPase Secretion-Associated and Ras-related protein 1 (Sar1) is activated by the guanine nucleotide exchange factor Sec12, causing Sar1-GTP to insert into the ER membrane. This recruits the Sec23/24 complex for cargo selection and then the Sec13/31 complex, which forms the outer coat and drives vesicle scission from the ER [
69]. (<b>B</b>) TANGO1 and cTAGE5 form a scaffold at ER exit sites (ERES), coordinating the recruitment of COPII components and facilitating cargo loading, particularly for large cargo like collagen. TANGO1 binds Sec23/24 and interacts with collagen, while cTAGE5 stabilizes Sar1-GTP and supports COPII assembly nucleation through its interaction with Sec12 [
49,
88] CC1—Coiled-coil domain 1, CC2—Coiled-coil domain; SH3—Src homology 3; PRD—Proline rich domain. (<b>C</b>) TANGO1 family proteins help form a transient tunnel or membrane continuity between the ER and the ER-Golgi intermediate compartment (ERGIC), enabling the direct transfer of bulky cargo like collagens. This tunnel bypasses conventional vesicle budding [
70,
75], allowing the export of large extracellular matrix proteins that exceed typical COPII vesicle size.
4. TANGO1-Regulated Collagen Export by Other Cell Types
TANGO1 is thought to be broadly expressed across nearly all cell types in animals based on studies in Drosophila and mammals. In Drosophila, its expression correlates loosely with secretory activity, showing particularly high levels in salivary gland cells—which secrete mucin-like glue proteins—and in the fat body, which produces the organism’s only collagen, Viking [
84,
89,
90,
91]. In mammalian fibroblasts, TANGO1 is essential for the export of numerous extracellular matrix (ECM) proteins, including procollagens I, III, V, VI, and XII, as well as fibrillin, fibronectin, and versican, supporting matrix assembly during development and tissue repair [
54]. This dependence on TANGO1 for ECM secretion is observed in multiple cell types and physiological contexts. In chondrocytes, TANGO1 deficiency disrupts collagen secretion and results in skeletal dysplasia, emphasizing its role in cartilage formation [
81,
82,
84]. In cultured RPE1 cells, loss of TANGO1 and its partner cTAGE5 significantly reduces secretion of many ECM components [
92]. In hepatic stellate cells and myofibroblasts, TANGO1 is upregulated in response to fibrotic signals and promotes collagen deposition [
93], directly linking it to pathological matrix accumulation. Similarly, in osteoblasts, TANGO1 supports the export of type I collagen, which is critical for bone matrix production. Although ubiquitously expressed, TANGO1’s functional necessity is heightened in cells with high or inducible secretory demands, suggesting a context-dependent role shaped by cargo load and secretory architecture. Further studies are needed to systematically define the cell- and tissue-specific expression and regulation of this protein.
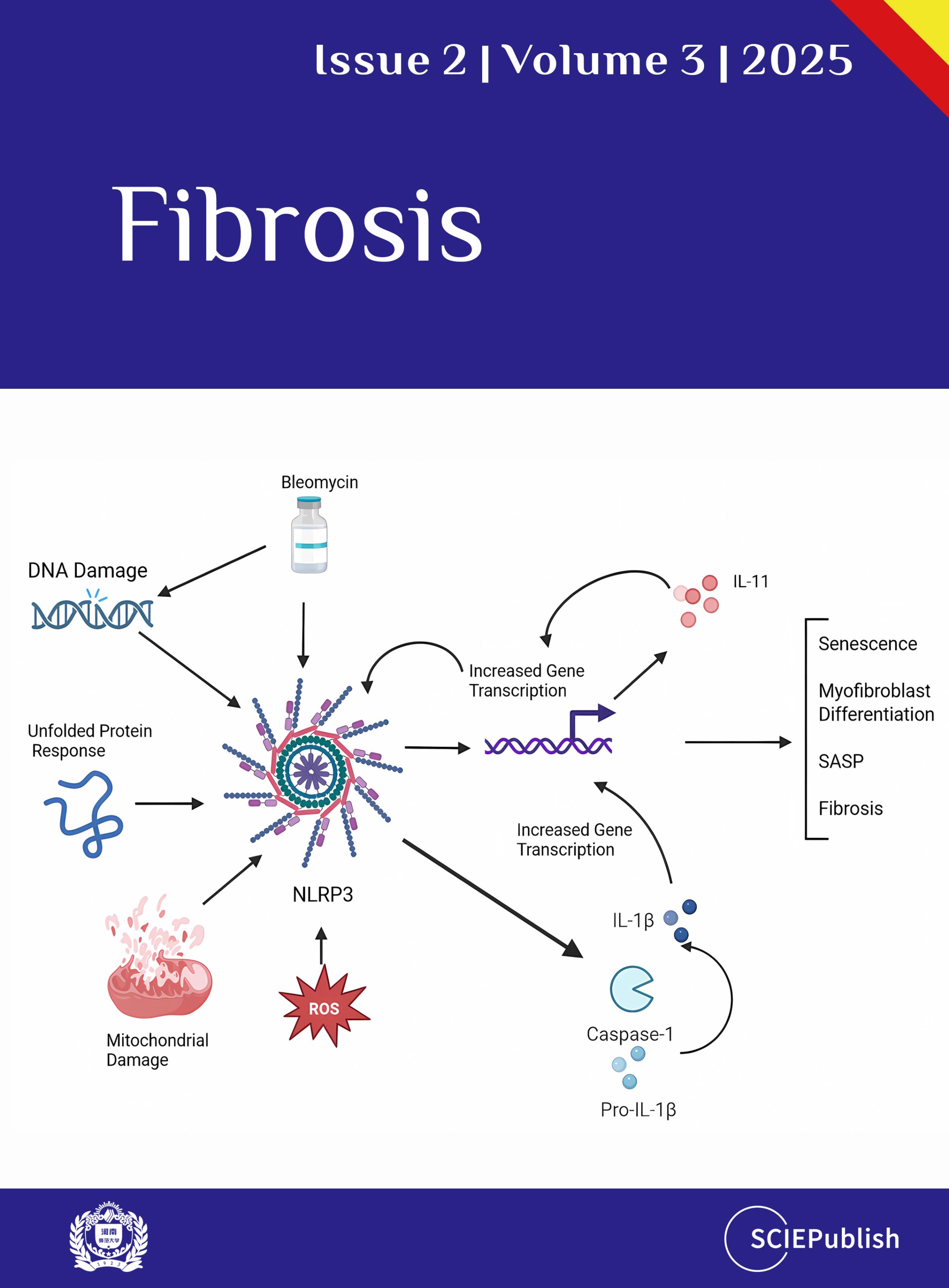
5. Signal Transduction Pathways Regulating TANGO1 Expression
TANGO1 expression is transcriptionally upregulated by ER stress via the inositol-requiring enzyme 1 (IRE1)–X-box binding protein 1 (XBP1) arm of the unfolded protein response (UPR) [
94], likely to enhance secretory capacity under load [
95]. Inflammatory stimuli also induce
MIA3 expression through caspase-1 activation and downstream IL-1 and TGF-β signalling [
93]. TGF-β alone can drive
MIA3 transcription via Smad2/3 binding to regulatory elements, particularly in fibrotic settings [
96]. TANGO1’s upregulation in certain fibrotic cells, including hepatic stellate cells and systemic sclerosis (SSc) fibroblasts, likely reflects increased ER demand from ECM hypersecreting myofibroblasts [
93]. Inflammatory signaling regulates TANGO1 expression. Caspase-1, the TGF-β receptor, and the IL-1 receptor all influence its levels. Blocking IL-1 reduced TANGO1 without affecting collagen expression, suggesting post-transcriptional control. In contrast, inhibiting TGF-β lowered both collagen and TANGO1, implying either a shared transcriptional program or feedback from secretory load. Notably, these changes selectively impaired the secretion of large proteins, while smaller cargoes were largely unaffected. The coordinated regulation of TANGO1 and collagen hints at functional coupling between cargo and export machinery, which may offer new entry points for therapeutic intervention in fibrosis [
97]. Insulin and IGF-1 signalling may influence expression through PI3K/AKT and MAPK pathways, though mechanistic links remain incomplete. Post-transcriptionally, TANGO1 is repressed by multiple microRNAs, including miR-125b, miR-30a, and miR-222, which reduce
MIA3 expression and promote proliferation and invasion in cancer models [
98,
99,
100]. Circadian regulation of TANGO1 mRNA suggests a coupling between secretion and diurnal cycles, though the underlying mechanism is not fully resolved [
101].
At the post-translational level, TANGO1 function is modulated by glycosylation [
83]. Its activity at ER exit sites is also dynamically controlled by Casein Kinase 1-mediated phosphorylation and Protein Phosphatase 1-dependent dephosphorylation, linking it to ER export site turnover [
102].
Despite these advances, key regulatory aspects remain undefined. The differential control of TANGO1-long and TANGO1-short isoforms has not been characterized. It is unknown how
MIA3 expression is modulated during transitions into hypersecretory states, such as during plasma cell differentiation or myofibroblast activation. Moreover, the cell- and tissue-specific regulation of TANGO1 remains largely unexplored. A systematic understanding of how secretory demands are matched to TANGO1 isoform expression and activity is still lacking, representing an exciting future for how cells and the ECM reciprocally control tissue assembly.
By integrating cargo selection, membrane remodeling, and trafficking, the TANGO1 family acts as master organizers of ERES, particularly for the enhanced secretory capacity imposed by bulky ECM proteins [
103]. Understanding their function illuminates core principles of membrane traffic and opens up new possibilities for targeting secretion in disease.
6. Therapeutic Implications
A defining feature of fibrotic disease is the excessive accumulation of extracellular matrix (ECM) components. While ECM levels are shaped by both synthesis and degradation, the production and secretion of matrix proteins are prerequisites for their pathological build-up. Although proteolytic degradation of ECM has long been recognized as important in fibrosis [
14,
104], targeting ECM synthesis is challenging due to its molecule-specific gene regulation and the complex biosynthetic steps involving post-translational modification and assembly.
In contrast, TANGO1 is a core component of the secretory pathway that governs the export of bulky cargoes, including many ECM proteins. Because it controls a common bottleneck for secretion, TANGO1 presents an attractive target for reducing matrix deposition across various fibrotic contexts. Modulating secretion could offer a general therapeutic strategy, independent of the specific fibrotic trigger or cytokine environment.
TANGO1 deletion blocked the secretion of collagen I in a mouse model of liver fibrosis. The TANGO1 deletion led to intracellular collagen retention, ER stress, and activation of the UPR [
54], which in turn induced TANGO1 expression via TGF-β1 signaling and the transcription factor XBP1 [
94]. ER export has long seemed “undruggable” because it is essential for cell viability. However, more recent studies have achieved some cargo specificity by inhibiting specific interfaces between interacting ERES proteins [
105,
106].
Recent advances in structural prediction and high-resolution mapping of protein complexes now allow precise identification of interaction surfaces within multi-protein assemblies. As we gain structural clarity on the interfaces that mediate cargo recognition, coat recruitment, and membrane tethering, new therapeutic possibilities emerge. Such precision offers a path forward for selectively controlling collagen export without broadly disrupting the secretory pathway, and may extend to other large cargoes and disease contexts in the future.
This strategy proved useful, as mapping interactions between TANGO1, cTAGE5, and their partners revealed specific domains critical for collagen export. Blocking these interactions provides a means to inhibit collagen secretion selectively. Membrane-permeant peptide inhibitors have been designed to disrupt interactions between TANGO1 and cTAGE5 (). These inhibitors mimic TANGO1 and cTAGE5’s CC2 domains and are conjugated to cell-penetrating peptides (CPPs) for intracellular delivery [
107,
108]. By precisely targeting the TANGO1-cTAGE5 interface, these peptides modulate ER export of ECM proteins without broadly disrupting secretion [
54].
In primary fibroblasts, isolated from both healthy individuals and those with scleroderma, these inhibitors markedly reduce the secretion of ECM proteins. Retained collagens are likely cleared by ER-phagy or proteasomal degradation, preventing intracellular accumulation [
109,
110]. In a zebrafish wound-healing model, treatment with peptide inhibitors decreases granulation tissue formation. By selectively blocking TANGO1 function, this approach provides a targeted strategy to control collagen secretion, thereby opening a new avenue for therapeutic intervention in fibrotic diseases.
.
ECM Proteins with Secretion Altered by TANGO1/cTAGE5 Inhibition [54].
| Collagen α1(I) |
Fibrillin-1 |
| Collagen α2(I) |
Fibronectin |
| Collagen α1(XII) |
Extracellular Matrix Protein-1 |
| Collagen α1(V) |
Laminin α4 |
| Collagen α3(VI) |
Collagen IV |
| Collagen α2(VI) |
|
However, systemic inhibition of TANGO1 is not without risks. Its essential role in secretion is underscored by the severe developmental defects seen in patients with TANGO1 mutations. Any therapeutic strategy must therefore allow for precise, reversible, and tissue-specific modulation. This could involve transient knockdown approaches—such as siRNAs—or new molecules that disrupt specific protein-protein interactions, like the TANGO1–cTAGE5 complexes.
Local delivery might provide a safer route. Topical or aerosol formulations targeting TANGO1 in accessible organs—such as the skin or lung—could suppress fibrosis while limiting systemic effects. This approach could be used to treat pulmonary fibrosis, excessive granulation tissue in wounds, or reduce scarring after surgery. It may also hold promise in localized fibrotic skin disorders, including scleroderma, lichen sclerosus et atrophicus, or chronic sclerodermiform graft-versus-host disease.
Collagen deposition is a defining molecular event in the development of fibrosis. Its accumulation stiffens tissue, disrupts architecture, and drives organ failure. In animal models, reducing collagen secretion consistently leads to attenuated fibrosis and preserved function, underscoring a causal role. TANGO1, an essential organizer of collagen export at ER exit sites, is now a tractable target. Recent studies have demonstrated that specific inhibitors of TANGO1 reduce collagen secretion
in vivo, with marked decreases in fibrotic burden and no overt toxicity. These results point to a direct, mechanistic intervention—interfering with the export of the principal fibrotic substrate—as a viable therapeutic strategy.
Statement of the Use of Generative AI and AI-Assisted Technologies in the Writing Process
During the preparation of this manuscript, the authors used ChatGPT in order to improve the clarity and readability of the text. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the published article.
Acknowledgements
The authors thank Vivek Malhotra (CRG Barcelona) for continued stimulating discussion.
Author Contributions
Conceptualization, B.E., G.S., I.R., T.K.; Writing—original draft preparation, B.E., G.S., I.R., T.K.; Writing—review and editing, O.T, A.B., J.N., I.N., G.S., B.E., I.R., T.K.; Visualization, O.T.; Funding acquisition, I.R., J.N., G.S., T.K.
Ethics Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Funding
Parts of this work were supported by Deutsche Forschungsgemeinschaft (German Research Foundation) through KR 558/17 and SE 115/7-1 (project ID 468236352 to T.K. and G.S.) and through the Research Unit Grant FOR2722 (NU 467/1-1 and DE 3170/1-1; project ID 384170921 to J.N.). JN acknowledges support by the Center for Molecular Medicine Cologne (CMMC) through the Individual Project Funding Program (Project C10) and the Career Advancement Program (Project CAP31) (to J.N.). T.K. is supported by CECAD and CMMC (SRG). I.R. acknowledges the support of Fondation pour la Recherche Médicale (grant AJE202210016216) and the ANR (MatSec).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1.
Distler JHW, Gyorfi AH, Ramanujam M, Whitfield ML, Konigshoff M, Lafyatis R. Shared and distinct mechanisms of fibrosis.
Nat. Rev. Rheumatol. 2019,
15, 705–730. doi:10.1038/s41584-019-0322-7.
[Google Scholar]
2.
Varga J, Abraham D. Systemic sclerosis: a prototypic multisystem fibrotic disorder.
J. Clin. Invest. 2007,
117, 557–567. doi:10.1172/JCI31139.
[Google Scholar]
3.
Gabrielli A, Avvedimento EV, Krieg T. Scleroderma.
N. Engl. J. Med. 2009,
360, 1989–2003. doi:10.1056/NEJMra0806188.
[Google Scholar]
4.
Allanore Y, Simms R, Distler O, Trojanowska M, Pope J, Denton CP, et al. Systemic sclerosis.
Nat. Rev. Dis. Primers. 2015,
1, 15002. doi:10.1038/nrdp.2015.2.
[Google Scholar]
5.
Eckes B, Wang F, Moinzadeh P, Hunzelmann N, Krieg T. Pathophysiological mechanisms in sclerosing skin diseases.
Front. Med. 2017,
4, 120. doi:10.3389/fmed.2017.00120.
[Google Scholar]
6.
Rockey DC, Bell PD, Hill JA. Fibrosis--a common pathway to organ injury and failure.
N. Engl. J. Med. 2015,
372, 1138–1149. doi:10.1056/NEJMra1300575.
[Google Scholar]
7.
Krieg T, Aumailley M. The extracellular matrix of the dermis: flexible structures with dynamic functions.
Exp. Dermatol. 2011,
20, 689–695. doi:10.1111/j.1600-0625.2011.01313.x.
[Google Scholar]
8.
Eckes B, Nischt R, Krieg T. Cell-matrix interactions in dermal repair and scarring.
Fibrogenesis Tissue Repair 2010,
3, 4. doi:10.1186/1755-1536-3-4.
[Google Scholar]
9.
Naba A, Clauser KR, Ding H, Whittaker CA, Carr SA, Hynes RO. The extracellular matrix: Tools and insights for the "omics" era.
Matrix Biol. 2016,
49, 10–24. doi:10.1016/j.matbio.2015.06.003.
[Google Scholar]
10.
Hynes RO, Naba A. Overview of the matrisome--an inventory of extracellular matrix constituents and functions.
Cold Spring Harb Perspect Biol 2012,
4, a004903. doi:10.1101/cshperspect.a004903.
[Google Scholar]
11.
Hynes RO. The extracellular matrix: not just pretty fibrils.
Science 2009,
326, 1216–1219. doi:10.1126/science.1176009.
[Google Scholar]
12.
Bruckner P. Suprastructures of extracellular matrices: paradigms of functions controlled by aggregates rather than molecules.
Cell Tissue Res. 2010,
339, 7–18. doi:10.1007/s00441-009-0864-0.
[Google Scholar]
13.
Charras G, Sahai E. Physical influences of the extracellular environment on cell migration.
Nat. Rev. Mol. Cell. Biol. 2014,
15, 813–824. doi:10.1038/nrm3897.
[Google Scholar]
14.
Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease.
Nat. Rev. Mol. Cell. Biol. 2014,
15, 786–801. doi:10.1038/nrm3904.
[Google Scholar]
15.
Sawant M, Hinz B, Schonborn K, Zeinert I, Eckes B, Krieg T, et al. A story of fibers and stress: Matrix-embedded signals for fibroblast activation in the skin.
Wound Repair Regen. 2021,
29, 515–530. doi:10.1111/wrr.12950.
[Google Scholar]
16.
Ricard-Blum S, Ruggiero F. The collagen superfamily: from the extracellular matrix to the cell membrane.
Pathol Biol (Paris) 2005,
53, 430–442. doi:10.1016/j.patbio.2004.12.024.
[Google Scholar]
17.
Kadler KE, Baldock C, Bella J, Boot-Handford RP. Collagens at a glance.
J. Cell Sci. 2007,
120, 1955–1958. doi:10.1242/jcs.03453.
[Google Scholar]
18.
Ricard-Blum S, Baffet G, Theret N. Molecular and tissue alterations of collagens in fibrosis.
Matrix Biol. 2018,
68–69, 122–149. doi:10.1016/j.matbio.2018.02.004.
[Google Scholar]
19.
Hedtke T, Schrader CU, Heinz A, Hoehenwarter W, Brinckmann J, Groth T, et al. A comprehensive map of human elastin cross-linking during elastogenesis.
FEBS J. 2019,
286, 3594–3610. doi:10.1111/febs.14929.
[Google Scholar]
20.
Sengle G, Sakai LY. The fibrillin microfibril scaffold: A niche for growth factors and mechanosensation?
Matrix Biol. 2015,
47, 3–12. doi:10.1016/j.matbio.2015.05.002.
[Google Scholar]
21.
Adamo CS, Zuk AV, Sengle G. The fibrillin microfibril/elastic fibre network: A critical extracellular supramolecular scaffold to balance skin homoeostasis.
Exp. Dermatol. 2021,
30, 25–37. doi:10.1111/exd.14191.
[Google Scholar]
22.
Godwin ARF, Dajani R, Zhang X, Thomson J, Holmes DF, Adamo CS, et al. Fibrillin microfibril structure identifies long-range effects of inherited pathogenic mutations affecting a key regulatory latent TGFbeta-binding site.
Nat. Struct. Mol. Biol. 2023,
30, 608–618. doi:10.1038/s41594-023-00950-8.
[Google Scholar]
23.
Schiavinato A, Keene DR, Wohl AP, Corallo D, Colombatti A, Wagener R, et al. Targeting of EMILIN-1 and EMILIN-2 to Fibrillin Microfibrils Facilitates their Incorporation into the Extracellular Matrix.
J. Invest. Dermatol. 2016,
136, 1150–1160. doi:10.1016/j.jid.2016.02.021.
[Google Scholar]
24.
Schiavinato A, Marcous F, Zuk AV, Keene DR, Tufa SF, Mosquera LM, et al. New insights into the structural role of EMILINs within the human skin microenvironment.
Sci. Rep. 2024,
14, 30345. doi:10.1038/s41598-024-81509-5.
[Google Scholar]
25.
Przyklenk M, Georgieva VS, Metzen F, Mostert S, Kobbe B, Callewaert B, et al. LTBP1 promotes fibrillin incorporation into the extracellular matrix.
Matrix Biol. 2022,
110, 60–75. doi:10.1016/j.matbio.2022.04.004.
[Google Scholar]
26.
Hynes RO. Integrins: bidirectional, allosteric signaling machines.
Cell 2002,
110, 673–687. doi:10.1016/s0092-8674(02)00971-6.
[Google Scholar]
27.
Barczyk M, Carracedo S, Gullberg D. Integrins.
Cell Tissue Res. 2010,
339, 269–280. doi:10.1007/s00441-009-0834-6.
[Google Scholar]
28.
Schulz JN, Plomann M, Sengle G, Gullberg D, Krieg T, Eckes B. New developments on skin fibrosis—Essential signals emanating from the extracellular matrix for the control of myofibroblasts.
Matrix Biol. 2018,
68–69, 522–532. doi:10.1016/j.matbio.2018.01.025.
[Google Scholar]
29.
Sawant M, Wang F, Koester J, Niehoff A, Nava MM, Lundgren-Akerlund E, et al. Ablation of integrin-mediated cell-collagen communication alleviates fibrosis.
Ann. Rheum. Dis. 2023,
82, 1474–1486. doi:10.1136/ard-2023-224129.
[Google Scholar]
30.
Coelho NM, McCulloch CA. Mechanical signaling through the discoidin domain receptor 1 plays a central role in tissue fibrosis.
Cell Adh. Migr. 2018,
12, 348–362. doi:10.1080/19336918.2018.1448353.
[Google Scholar]
31.
Hinz B, Lagares D. Evasion of apoptosis by myofibroblasts: a hallmark of fibrotic diseases.
Nat. Rev. Rheumatol. 2020,
16, 11–31. doi:10.1038/s41584-019-0324-5.
[Google Scholar]
32.
Monboisse JC, Oudart JB, Ramont L, Brassart-Pasco S, Maquart FX. Matrikines from basement membrane collagens: a new anti-cancer strategy.
Biochim. Biophys. Acta 2014,
1840, 2589–2598. doi:10.1016/j.bbagen.2013.12.029.
[Google Scholar]
33.
Brassart-Pasco S, Senechal K, Thevenard J, Ramont L, Devy J, Di Stefano L, et al. Tetrastatin, the NC1 domain of the alpha4(IV) collagen chain: a novel potent anti-tumor matrikine.
PLoS One 2012,
7, e29587. doi:10.1371/journal.pone.0029587.
[Google Scholar]
34.
Ricard-Blum S, Ballut L. Matricryptins derived from collagens and proteoglycans.
Front. Biosci. 2011,
16, 674–697. doi:10.2741/3712.
[Google Scholar]
35.
Gaggar A, Weathington N. Bioactive extracellular matrix fragments in lung health and disease.
J. Clin. Invest. 2016,
126, 3176–3184. doi:10.1172/JCI83147.
[Google Scholar]
36.
de Castro Bras LE, Frangogiannis NG. Extracellular matrix-derived peptides in tissue remodeling and fibrosis.
Matrix Biol. 2020,
91–92, 176–187. doi:10.1016/j.matbio.2020.04.006.
[Google Scholar]
37.
Saharinen J, Keski-Oja J. Specific sequence motif of 8-Cys repeats of TGF-beta binding proteins, LTBPs, creates a hydrophobic interaction surface for binding of small latent TGF-beta.
Mol. Biol. Cell 2000,
11, 2691–2704. doi:10.1091/mbc.11.8.2691.
[Google Scholar]
38.
Zilberberg L, Todorovic V, Dabovic B, Horiguchi M, Courousse T, Sakai LY, et al. Specificity of latent TGF-beta binding protein (LTBP) incorporation into matrix: role of fibrillins and fibronectin.
J. Cell Physiol. 2012,
227, 3828–3836. doi:10.1002/jcp.24094.
[Google Scholar]
39.
Horiguchi M, Ota M, Rifkin DB. Matrix control of transforming growth factor-beta function.
J. Biochem. 2012,
152, 321–329. doi:10.1093/jb/mvs089.
[Google Scholar]
40.
Ono RN, Sengle G, Charbonneau NL, Carlberg V, Bachinger HP, Sasaki T, et al. Latent transforming growth factor beta-binding proteins and fibulins compete for fibrillin-1 and exhibit exquisite specificities in binding sites.
J. Biol. Chem. 2009,
284, 16872–16881. doi:10.1074/jbc.M809348200.
[Google Scholar]
41.
Isogai Z, Ono RN, Ushiro S, Keene DR, Chen Y, Mazzieri R, et al. Latent transforming growth factor beta-binding protein 1 interacts with fibrillin and is a microfibril-associated protein.
J. Biol. Chem. 2003,
278, 2750–2757. doi:10.1074/jbc.M209256200.
[Google Scholar]
42.
Loeys BL, Gerber EE, Riegert-Johnson D, Iqbal S, Whiteman P, McConnell V, et al. Mutations in fibrillin-1 cause congenital scleroderma: stiff skin syndrome.
Sci. Transl. Med. 2010,
2, 23ra20. doi:10.1126/scitranslmed.3000488.
[Google Scholar]
43.
Zigrino P, Sengle G. Fibrillin microfibrils and proteases, key integrators of fibrotic pathways.
Adv. Drug Deliv. Rev. 2019,
146, 3–16. doi:10.1016/j.addr.2018.04.019.
[Google Scholar]
44.
Wipff PJ, Rifkin DB, Meister JJ, Hinz B. Myofibroblast contraction activates latent TGF-beta1 from the extracellular matrix.
J. Cell Biol. 2007,
179, 1311–1323. doi:10.1083/jcb.200704042.
[Google Scholar]
45.
Wipff PJ, Hinz B. Integrins and the activation of latent transforming growth factor beta1 - an intimate relationship.
Eur. J. Cell. Biol. 2008,
87, 601–615. doi:10.1016/j.ejcb.2008.01.012.
[Google Scholar]
46.
Margadant C, Sonnenberg A. Integrin-TGF-beta crosstalk in fibrosis, cancer and wound healing.
EMBO Rep. 2010,
11, 97–105. doi:10.1038/embor.2009.276.
[Google Scholar]
47.
Frangogiannis N. Transforming growth factor-beta in tissue fibrosis.
J. Exp. Med. 2020,
217, e20190103. doi:10.1084/jem.20190103.
[Google Scholar]
48.
Malhotra V, Erlmann P. The pathway of collagen secretion.
Annu. Rev. Cell. Dev. Biol. 2015,
31, 109–124. doi:10.1146/annurev-cellbio-100913-013002.
[Google Scholar]
49.
Saito K, Yamashiro K, Ichikawa Y, Erlmann P, Kontani K, Malhotra V, et al. cTAGE5 mediates collagen secretion through interaction with TANGO1 at endoplasmic reticulum exit sites.
Mol. Biol. Cell 2011,
22, 2301–2308. doi:10.1091/mbc.E11-02-0143.
[Google Scholar]
50.
Raote I, Malhotra V. Protein transport by vesicles and tunnels.
J. Cell Biol. 2019,
218, 737–739. doi:10.1083/jcb.201811073.
[Google Scholar]
51.
Raote I, Ernst AM, Campelo F, Rothman JE, Pincet F, Malhotra V. TANGO1 membrane helices create a lipid diffusion barrier at curved membranes.
Elife 2020,
9. doi:10.7554/eLife.57822.
[Google Scholar]
52.
Raote I, Chabanon M, Walani N, Arroyo M, Garcia-Parajo MF, Malhotra V, et al. A physical mechanism of TANGO1-mediated bulky cargo export.
Elife 2020,
9. doi:10.7554/eLife.59426.
[Google Scholar]
53.
Raote I, Saxena S, Malhotra V. Sorting and Export of Proteins at the Endoplasmic Reticulum.
Cold Spring Harb. Perspect. Biol. 2023,
15. doi:10.1101/cshperspect.a041258.
[Google Scholar]
54.
Raote I, Rosendahl AH, Hakkinen HM, Vibe C, Kucukaylak I, Sawant M, et al. TANGO1 inhibitors reduce collagen secretion and limit tissue scarring.
Nat. Commun. 2024,
15, 3302. doi:10.1038/s41467-024-47004-1.
[Google Scholar]
55.
Hulmes DJ. Building collagen molecules, fibrils, and suprafibrillar structures.
J. Struct. Biol. 2002,
137, 2–10. doi:10.1006/jsbi.2002.4450.
[Google Scholar]
56.
Akhurst RJ, Hata A. Targeting the TGFbeta signalling pathway in disease.
Nat. Rev. Drug Discov. 2012,
11, 790–811. doi:10.1038/nrd3810.
[Google Scholar]
57.
Henderson NC, Arnold TD, Katamura Y, Giacomini MM, Rodriguez JD, McCarty JH, et al. Targeting of alphav integrin identifies a core molecular pathway that regulates fibrosis in several organs.
Nat. Med. 2013,
19, 1617–1624. doi:10.1038/nm.3282.
[Google Scholar]
58.
Radovanac K, Morgner J, Schulz JN, Blumbach K, Patterson C, Geiger T, et al. Stabilization of integrin-linked kinase by the Hsp90-CHIP axis impacts cellular force generation, migration and the fibrotic response.
EMBO J. 2013,
32, 1409–1424. doi:10.1038/emboj.2013.90.
[Google Scholar]
59.
Zhou Y, Huang X, Hecker L, Kurundkar D, Kurundkar A, Liu H, et al. Inhibition of mechanosensitive signaling in myofibroblasts ameliorates experimental pulmonary fibrosis.
J. Clin. Invest. 2013,
123, 1096–1108. doi:10.1172/JCI66700.
[Google Scholar]
60.
Kim I, Mogford JE, Witschi C, Nafissi M, Mustoe TA. Inhibition of prolyl 4-hydroxylase reduces scar hypertrophy in a rabbit model of cutaneous scarring.
Wound Repair Regen. 2003,
11, 368–372. doi:10.1046/j.1524-475x.2003.11509.x.
[Google Scholar]
61.
Franklin TJ. Therapeutic approaches to organ fibrosis.
Int. J. Biochem. Cell. Biol. 1997,
29, 79–89. doi:10.1016/s1357-2725(96)00121-5.
[Google Scholar]
62.
Yang J, Savvatis K, Kang JS, Fan P, Zhong H, Schwartz K, et al. Targeting LOXL2 for cardiac interstitial fibrosis and heart failure treatment.
Nat. Commun. 2016,
7, 13710. doi:10.1038/ncomms13710.
[Google Scholar]
63.
Ikenaga N, Peng ZW, Vaid KA, Liu SB, Yoshida S, Sverdlov DY, et al. Selective targeting of lysyl oxidase-like 2 (LOXL2) suppresses hepatic fibrosis progression and accelerates its reversal.
Gut 2017,
66, 1697–1708. doi:10.1136/gutjnl-2016-312473.
[Google Scholar]
64.
Jun JI, Lau LF. Resolution of organ fibrosis.
J. Clin. Invest. 2018,
128, 97–107. doi:10.1172/JCI93563.
[Google Scholar]
65.
Hamanaka RB, Mutlu GM. The role of metabolic reprogramming and de novo amino acid synthesis in collagen protein production by myofibroblasts: implications for organ fibrosis and cancer.
Amino Acids 2021,
53, 1851–1862. doi:10.1007/s00726-021-02996-8.
[Google Scholar]
66.
Lagares D, Santos A, Grasberger PE, Liu F, Probst CK, Rahimi RA, et al. Targeted apoptosis of myofibroblasts with the BH3 mimetic ABT-263 reverses established fibrosis.
Sci. Transl. Med. 2017,
9. doi:10.1126/scitranslmed.aal3765.
[Google Scholar]
67.
Aghajanian H, Kimura T, Rurik JG, Hancock AS, Leibowitz MS, Li L, et al. Targeting cardiac fibrosis with engineered T cells.
Nature 2019,
573, 430–433. doi:10.1038/s41586-019-1546-z.
[Google Scholar]
68.
Ishikawa Y, Bachinger HP. A molecular ensemble in the rER for procollagen maturation.
Biochim. Biophys. Acta 2013,
1833, 2479–2491. doi:10.1016/j.bbamcr.2013.04.008.
[Google Scholar]
69.
Downes KW, Zanetti G. Mechanisms of COPII coat assembly and cargo recognition in the secretory pathway.
Nat. Rev. Mol. Cell. Biol. 2025. doi:10.1038/s41580-025-00839-y.
[Google Scholar]
70.
Raote I, Malhotra V. Tunnels for protein export from the endoplasmic reticulum.
Annu. Rev. Biochem. 2021,
90, 605–630. doi:10.1146/annurev-biochem-080120-022017.
[Google Scholar]
71.
Bard F, Casano L, Mallabiabarrena A, Wallace E, Saito K, Kitayama H, et al. Functional genomics reveals genes involved in protein secretion and Golgi organization.
Nature 2006,
439, 604–607. doi:10.1038/nature04377.
[Google Scholar]
72.
Saito K, Chen M, Bard F, Chen S, Zhou H, Woodley D, et al. TANGO1 facilitates cargo loading at endoplasmic reticulum exit sites.
Cell 2009,
136, 891–902. doi:10.1016/j.cell.2008.12.025.
[Google Scholar]
73.
Feng Z, Yang K, Pastor-Pareja JC. Tales of the ER-Golgi frontier: Drosophila-centric considerations on Tango1 function.
Front. Cell. Dev. Biol. 2020,
8, 619022. doi:10.3389/fcell.2020.619022.
[Google Scholar]
74.
Raote I, Ortega Bellido M, Pirozzi M, Zhang C, Melville D, Parashuraman S, et al. TANGO1 assembles into rings around COPII coats at ER exit sites.
J. Cell Biol. 2017,
216, 901–909. doi:10.1083/jcb.201608080.
[Google Scholar]
75.
Santos AJ, Raote I, Scarpa M, Brouwers N, Malhotra V. TANGO1 recruits ERGIC membranes to the endoplasmic reticulum for procollagen export.
Elife 2015,
4. doi:10.7554/eLife.10982.
[Google Scholar]
76.
Ma W, Goldberg J. TANGO1/cTAGE5 receptor as a polyvalent template for assembly of large COPII coats.
Proc. Natl. Acad. Sci. USA 2016,
113, 10061–10066. doi:10.1073/pnas.1605916113.
[Google Scholar]
77.
Arnolds O, Stoll R. Characterization of a fold in TANGO1 evolved from SH3 domains for the export of bulky cargos.
Nat. Commun. 2023,
14, 2273. doi:10.1038/s41467-023-37705-4.
[Google Scholar]
78.
Bunel L, Pincet L, Malhotra V, Raote I, Pincet F. A model for collagen secretion by intercompartmental continuities.
Proc. Natl. Acad. Sci. USA 2024,
121, e2310404120. doi:10.1073/pnas.2310404120.
[Google Scholar]
79.
Wilson DG, Phamluong K, Li L, Sun M, Cao TC, Liu PS, et al. Global defects in collagen secretion in a Mia3/TANGO1 knockout mouse.
J. Cell Biol. 2011,
193, 935–951. doi:10.1083/jcb.201007162.
[Google Scholar]
80.
Christen M, Booij-Vrieling H, Oksa-Minalto J, de Vries C, Kehl A, Jagannathan V, et al. MIA3 splice defect in cane corso dogs with dental-skeletal-retinal anomaly (DSRA).
Genes 2021,
12. doi:10.3390/genes12101497.
[Google Scholar]
81.
Brown AT, Peak RM, Smithson CW, Bell C. Dental abnormalities in two dental-skeletal-retinal anomaly-positive cane corso dogs: a case series.
J. Vet. Dent. 2024,
41, 409–423. doi:10.1177/08987564231215170.
[Google Scholar]
82.
Clark EM, Link BA. Complementary and divergent functions of zebrafish Tango1 and Ctage5 in tissue development and homeostasis.
Mol. Biol. Cell 2021,
32, 391–401. doi:10.1091/mbc.E20-11-0745.
[Google Scholar]
83.
Zhang L, Syed ZA, van Dijk Hard I, Lim JM, Wells L, Ten Hagen KG. O-glycosylation regulates polarized secretion by modulating Tango1 stability.
Proc. Natl. Acad. Sci. USA 2014,
111, 7296–7301. doi:10.1073/pnas.1322264111.
[Google Scholar]
84.
Tiwari P, Kumar A, Das RN, Malhotra V, VijayRaghavan K. A tendon cell specific RNAi screen reveals novel candidates essential for muscle tendon interaction.
PLoS One 2015,
10, e0140976. doi:10.1371/journal.pone.0140976.
[Google Scholar]
85.
Lekszas C, Foresti O, Raote I, Liedtke D, Konig EM, Nanda I, et al. Biallelic TANGO1 mutations cause a novel syndromal disease due to hampered cellular collagen secretion.
Elife 2020,
9. doi:10.7554/eLife.51319.
[Google Scholar]
86.
Pitman JL, Bonnet DJ, Curtiss LK, Gekakis N. Reduced cholesterol and triglycerides in mice with a mutation in Mia2, a liver protein that localizes to ER exit sites.
J. Lipid Res. 2011,
52, 1775–1786. doi:10.1194/jlr.M017277.
[Google Scholar]
87.
Santos AJ, Nogueira C, Ortega-Bellido M, Malhotra V. TANGO1 and Mia2/cTAGE5 (TALI) cooperate to export bulky pre-chylomicrons/VLDLs from the endoplasmic reticulum.
J. Cell Biol. 2016,
213, 343–354. doi:10.1083/jcb.201603072.
[Google Scholar]
88.
Saito K, Yamashiro K, Shimazu N, Tanabe T, Kontani K, Katada T. Concentration of Sec12 at ER exit sites via interaction with cTAGE5 is required for collagen export.
J. Cell Biol. 2014,
206, 751–762. doi:10.1083/jcb.201312062.
[Google Scholar]
89.
Liu M, Feng Z, Ke H, Liu Y, Sun T, Dai J, et al. Tango1 spatially organizes ER exit sites to control ER export.
J. Cell Biol. 2017,
216, 1035–1049. doi:10.1083/jcb.201611088.
[Google Scholar]
90.
Rios-Barrera LD, Sigurbjornsdottir S, Baer M, Leptin M. Dual function for Tango1 in secretion of bulky cargo and in ER-Golgi morphology.
Proc. Natl. Acad. Sci. USA 2017,
114, E10389–E10398. doi:10.1073/pnas.1711408114.
[Google Scholar]
91.
Lerner DW, McCoy D, Isabella AJ, Mahowald AP, Gerlach GF, Chaudhry TA, et al. A Rab10-dependent mechanism for polarized basement membrane secretion during organ morphogenesis.
Dev. Cell 2013,
24, 159–168. doi:10.1016/j.devcel.2012.12.005.
[Google Scholar]
92.
McCaughey J, Stevenson NL, Mantell JM, Neal CR, Paterson A, Heesom K, et al. A general role for TANGO1, encoded by MIA3, in secretory pathway organization and function.
J. Cell Sci. 2021,
134. doi:10.1242/jcs.259075.
[Google Scholar]
93.
Connolly LM, McFalls CM, McMahon IG, Bhat AM, Artlett CM. Caspase 1 enhances Transport and Golgi Organization Protein 1 expression to promote procollagen export from the endoplasmic reticulum in systemic sclerosis contributing to fibrosis.
Arthritis Rheumatol. 2023,
75, 1831–1841. doi:10.1002/art.42535.
[Google Scholar]
94.
Maiers JL, Kostallari E, Mushref M, deAssuncao TM, Li H, Jalan-Sakrikar N, et al. The unfolded protein response mediates fibrogenesis and collagen I secretion through regulating TANGO1 in mice.
Hepatology 2017,
65, 983–998. doi:10.1002/hep.28921.
[Google Scholar]
95.
Ishikawa T, Toyama T, Nakamura Y, Tamada K, Shimizu H, Ninagawa S, et al. UPR transducer BBF2H7 allows export of type II collagen in a cargo- and developmental stage-specific manner.
J. Cell Biol. 2017,
216, 1761–1774. doi:10.1083/jcb.201609100.
[Google Scholar]
96.
Chothani S, Schafer S, Adami E, Viswanathan S, Widjaja AA, Langley SR, et al. Widespread translational control of fibrosis in the human heart by RNA-binding proteins.
Circulation 2019,
140, 937–951. doi:10.1161/CIRCULATIONAHA.119.039596.
[Google Scholar]
97.
Artlett CA. The road well traveled: from inflammasomes to collagen export during fibrosis.
Sclerosis 2024,
2, 378–393. doi:10.3390/sclerosis2040025.
[Google Scholar]
98.
Du Q, Ye X, Lu SR, Li H, Liu HY, Zhai Q, et al. Exosomal miR-30a and miR-222 derived from colon cancer mesenchymal stem cells promote the tumorigenicity of colon cancer through targeting MIA3.
J. Gastrointest. Oncol. 2021,
12, 52–68. doi:10.21037/jgo-20-513.
[Google Scholar]
99.
Gao H, Cong X, Zhou J, Guan M. MicroRNA-222 influences migration and invasion through MIA3 in colorectal cancer.
Cancer Cell Int. 2017,
17, 78. doi:10.1186/s12935-017-0447-1.
[Google Scholar]
100.
Zhang X, Zhang F, Zhang C, Li J. miRNA-125b signaling ameliorates liver injury against obstructive jaundice-induced excessive fibrosis in experimental rats.
Yonsei Med. J. 2021,
62, 453–460. doi:10.3349/ymj.2021.62.5.453.
[Google Scholar]
101.
Chang J, Garva R, Pickard A, Yeung CC, Mallikarjun V, Swift J, et al. Circadian control of the secretory pathway maintains collagen homeostasis.
Nat. Cell. Biol. 2020,
22, 74–86. doi:10.1038/s41556-019-0441-z.
[Google Scholar]
102.
Maeda M, Komatsu Y, Saito K. Mitotic ER exit site disassembly and reassembly are regulated by the phosphorylation status of TANGO1.
Dev. Cell 2020,
55, 237–250 e235. doi:10.1016/j.devcel.2020.07.017.
[Google Scholar]
103.
Saito K, Maeda M. Not just a cargo receptor for large cargoes; an emerging role of TANGO1 as an organizer of ER exit sites.
J. Biochem. 2019,
166, 115–119. doi:10.1093/jb/mvz036.
[Google Scholar]
104.
Giannandrea M, Parks WC. Diverse functions of matrix metalloproteinases during fibrosis.
Dis. Model Mech. 2014,
7, 193–203. doi:10.1242/dmm.012062.
[Google Scholar]
105.
Forrester A, Rathjen SJ, Daniela Garcia-Castillo M, Bachert C, Couhert A, Tepshi L, et al. Functional dissection of the retrograde Shiga toxin trafficking inhibitor Retro-2.
Nat. Chem. Biol. 2020,
16, 327–336. doi:10.1038/s41589-020-0474-4.
[Google Scholar]
106.
Gomez-Navarro N, Maldutyte J, Poljak K, Peak-Chew SY, Orme J, Bisnett BJ, et al. Selective inhibition of protein secretion by abrogating receptor-coat interactions during ER export.
Proc. Natl. Acad. Sci. USA 2022,
119, e2202080119. doi:10.1073/pnas.2202080119.
[Google Scholar]
107.
Klimpel A, Stillger K, Wiederstein JL, Kruger M, Neundorf I. Cell-permeable CaaX-peptides affect K-Ras downstream signaling and promote cell death in cancer cells.
FEBS J. 2021,
288, 2911–2929. doi:10.1111/febs.15612.
[Google Scholar]
108.
Stillger K, Neundorf I. Cell-permeable peptide-based delivery vehicles useful for subcellular targeting and beyond.
Cell Signal. 2023,
109, 110796. doi:10.1016/j.cellsig.2023.110796.
[Google Scholar]
109.
Forrester A, De Leonibus C, Grumati P, Fasana E, Piemontese M, Staiano L, et al. A selective ER-phagy exerts procollagen quality control via a Calnexin-FAM134B complex.
EMBO J. 2019,
38. doi:10.15252/embj.201899847.
[Google Scholar]
110.
Omari S, Makareeva E, Roberts-Pilgrim A, Mirigian L, Jarnik M, Ott C, et al. Noncanonical autophagy at ER exit sites regulates procollagen turnover.
Proc. Natl. Acad. Sci. USA 2018,
115, E10099–E10108. doi:10.1073/pnas.1814552115.
[Google Scholar]
 Anna Bornikoel
2
Anna Bornikoel
2
 Julian Nüchel
3,4
Julian Nüchel
3,4
 Ines Neundorf
5
Ines Neundorf
5
 Gerhard Sengle
3,4,6,7,8
Gerhard Sengle
3,4,6,7,8
 Beate Eckes
2
Beate Eckes
2
 Ishier Raote
1,*
Ishier Raote
1,*
 Thomas Krieg
2,4,8,9,*
Thomas Krieg
2,4,8,9,*