1. Introduction
Patients with interstitial lung disease often wait a prolonged time before a diagnosis is established. Surveys and retrospective studies of patients with idiopathic pulmonary fibrosis (IPF) show a median diagnostic delay of 2.1 years [
1]. Similarly, 43% of patients with a self-reported diagnosis of interstitial lung disease (ILD) identified through the pulmonary fibrosis foundation reported a delay of at least one year, and 19% reported a delay of at least three years [
2]. The patient’s journey to diagnosis is also fraught with multiple misdiagnoses and invasive procedures during the evaluation [
2]. Patients similarly report a clear lack of information and resources on pulmonary fibrosis at the time of diagnosis [
3]. Efforts to improve the efficiency and accuracy of this diagnostic process are essential as delays have been associated with increased mortality for patients with IPF [
4] and rheumatoid arthritis associated with ILD [
5].
Once a concern for ILD exists, a presentation at a multidisciplinary discussion (MDD) to review all data is recommended [
6]. When patient history, laboratory evaluation, and radiographic findings are unrevealing, guidelines recommend considering obtaining a tissue biopsy to guide diagnosis and management [
7]. Although surgical lung biopsy (SLB) has been the standard method, a recent randomized clinical trial comparing TBLC and SLB has shown high concordance for both histopathological interpretation and MDD diagnoses [
8]. A subsequent randomized clinical trial comparing an upfront SLB diagnostic approach versus starting with TBLC followed by SLB if TBLC is inconclusive showed decreased chest tube duration, in-hospital length of stay, and similar diagnostic yields versus immediate SLB [
9]. Recommendations now advocate for the use of transbronchial lung cryobiopsy (TBLC) at experienced centers [
10] as when TBLC is used in conjunction with an MDD, it has comparable accuracy, decreased morbidity [
11,
12], and potential cost savings compared to SLB [
13,
14].
While outpatient lung biopsies have a low risk for complications [
15,
16,
17,
18], hospitalized patients have a higher historical risk. Studies of hospitalized patients with suspected ILD undergoing SLB may have significant morbidity post-procedure [
16,
17,
18], with mortality rates as high as 16% [
18]. In contrast, initial studies looking at inpatient TBLC appear to be relatively safe and effective in establishing a diagnosis [
19,
20]. While these studies are limited by a smaller sample size (
n = 17 inpatients [
19] and
n = 22 inpatients [
20]), inpatients had objectively higher levels of acuity based on comorbidities and American Society of Anesthesiology (ASA) scores, yet did not have a statistically significant increase in complications, including bleeding, pneumothorax, transfer to a higher level of care, or mortality [
19,
20].
While initial studies suggest that inpatient TBLC for newly identified ILD patients is safe, data evaluating the value of this intervention in impacting clinical management and establishing an ILD diagnosis is lacking. To help determine the potential benefit of inpatient TBLC on treatment initiation and wait times between identification of ILD on imaging and time to biopsy, we present a retrospective comparison of hospitalized and outpatients with newly identified ILD.
2. Methods
2.1. Study Cohort
All patients consecutively presenting to our interventional pulmonology (IP) clinic or inpatient consult service for evaluation of newly discovered ILD by high-resolution CT chest (HRCT) from November 2019 through May 2021 were consented for TBLC, underwent the procedure by one interventional pulmonologist in a dedicated bronchoscopy suite as previously described [
20], and were enrolled. During the study period, 77 total patients underwent TBLC, with 55 outpatients and 22 inpatients (). Ten (10) patients received an alternative diagnosis to ILD diagnosis (six outpatients, four inpatients), and 13 patients (nine outpatients, four inpatients) did not have treatment guided by TBLC results (medication initiation, adjustment, or cessation was not directly impacted by results of the TBLC procedure) and were thus excluded from the final analysis. The study was approved by the institutional review board of the Medical College of Wisconsin PRO00036023.
Demographic data, pulmonary function test (PFT) values, chest imaging pattern, final MDD diagnosis, time from consultation to biopsy and medical therapy change, and specific medical therapy changes, defined as medication initiation, adjustment, or cessation guided by TBLC results, were extracted from the medical record. Procedural information, including biopsy location, number of lobes biopsied, total biopsies performed, and procedure complications, including pneumothorax, bleeding severity, worsening respiratory status, change in level of care, and 30-day and 60-day mortality, were previously reported [
20]. Changes in medical therapy were the primary outcome. Time from consultation to biopsy and treatment initiation was the secondary outcome.
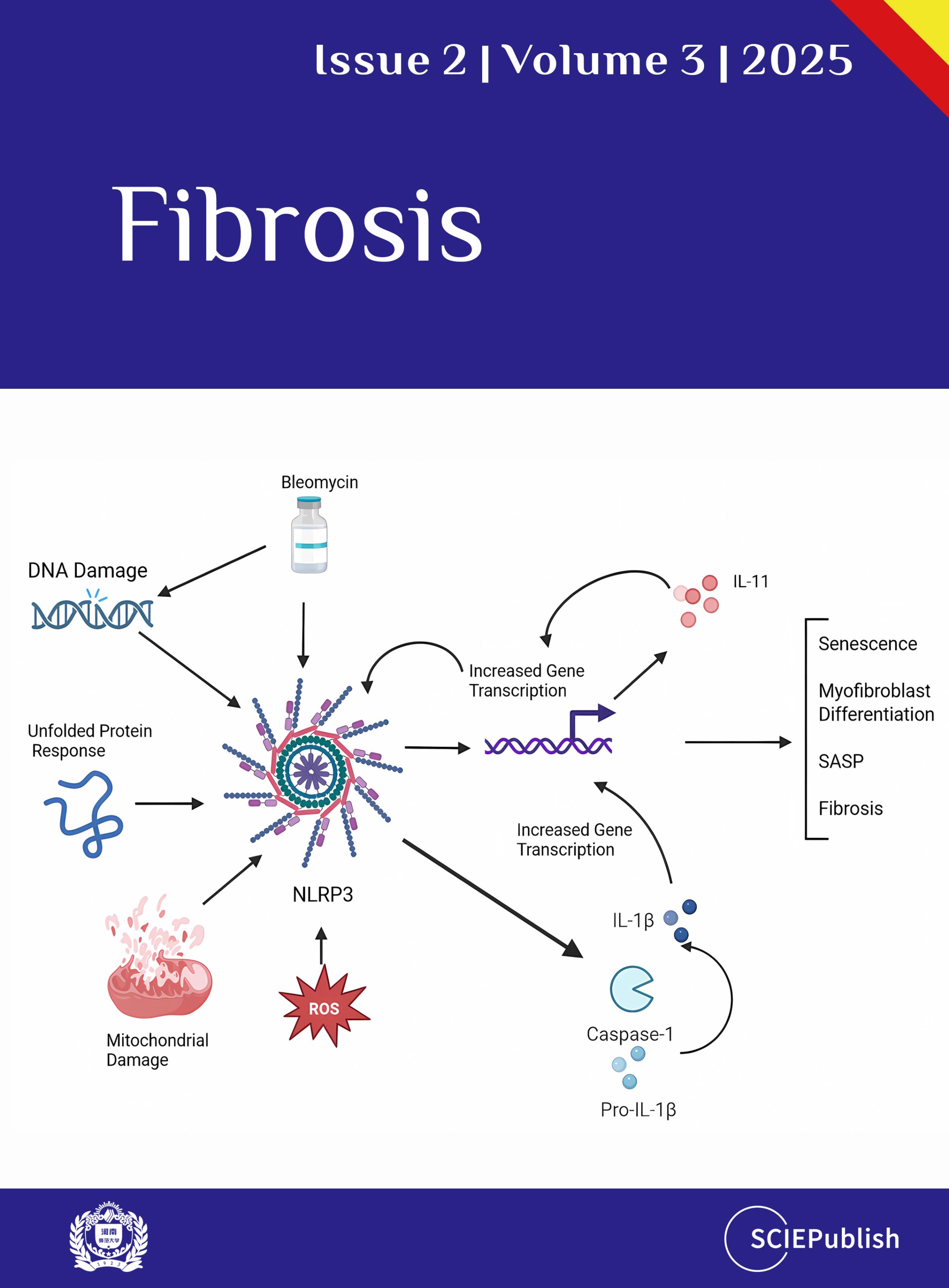
. Evaluation of patients undergoing transbronchial lung cryobiopsy and those included in the study. CPFE = combined pulmonary fibrosis and emphysema, ILD = interstitial lung disease, IPF = idiopathic pulmonary fibrosis, TBLC = transbronchial lung cryobiopsy.
Categorical variables were expressed as a number and percentages, and comparisons were performed with the Chi-square test or Fisher’s exact test. Continuous variables were expressed as mean with standard deviation or as an interquartile range with overall range, and comparisons were done with the Student’s
t-test or Mann-Whitney
u-test. All
p-values were two-sided, and
p < 0.05 was considered statistically significant. Statistical analysis was performed with SAS version 9.4 (SAS Institute, Cary, NC, USA).
3. Results
During the study period, 54 patients (40 outpatient, 14 inpatient) underwent TBLC, were diagnosed with ILD, and had treatment guided by the TBLC results. There were no significant differences in sex, race, PFTs, or chest imaging patterns between the groups (
). There was a significant difference in age between the groups, with inpatients being younger (59.4 ± 9.5 years) compared to outpatients (65.9 ± 11.3 years) (
p = 0.02). As described previously [
20], inpatients had a statistically significant increased ASA score (3.3 ± 0.48) compared to outpatients (3.0 ± 0.51) (
p = 0.0062) in addition to more total comorbidities (inpatient: 2.9 ± 1.6
vs. outpatient: 1.9 ± 1.2) (
p = 0.0070), including history of malignancy (inpatient: 68%
n = 15
vs. outpatient: 24%
n = 13) (
p = 0.0002) or history of transplant (inpatient: 31%
n = 7
vs. outpatient: 4%
n = 2) (
p = 0.0017). Inpatients were more likely to be treated with steroids for non-pulmonary disease (45%
n = 10
vs. 18%
n = 10) (
p = 0.0137), immunosuppressive therapy (36%
n = 8
vs. 13%
n = 7) (
p = 0.0266), and to require supplemental oxygen (55%
n = 12
vs. 18%
n = 10). Reasons for hospitalizations varied for inpatients, including hypoxic respiratory failure (
n = 11), COVID-19 pneumonia (
n = 2), dyspnea (
n = 2), interstitial lung disease (
n = 2), altered mental status (
n = 1), cholecystitis (
n = 1), pneumonia (
n = 1), pulmonary nodules (
n = 1), and severe sepsis (
n = 1).
.
Patient Characteristics.
| |
Outpatient |
Inpatient |
Total |
p Value |
| Age (mean ± SD) |
65.9 ± 11.3 |
59.4 ± 9.5 |
64.2 ± 11.1 |
0.02 |
| Sex (n, %) |
|
|
|
0.43 |
| Male |
18 (45.0%) |
8 (57.1%) |
26 (48.1%) |
|
| Female |
22 (55.0%) |
6 (42.9%) |
28 (51.9%) |
|
| Race (n, %) |
|
|
|
0.13 |
| Caucasian |
30 (75.0%) |
9 (64.3%) |
39 (72.2%) |
|
| Black |
6 (15.0%) |
2 (14.3%) |
8 (14.8%) |
|
| Hispanic |
1 (2.5%) |
3 (22.4%) |
4 (7.4%) |
|
| Asian |
3 (7.5%) |
0 (0.0%) |
3 (5.6%) |
|
| PFTs (mean ± SD) |
|
|
|
|
| FEV1 % predicted |
68.6 ± 16.4 |
67.7 ± 14.3 |
68.5 ± 16.0 |
0.89 |
| FVC % predicted |
65.3 ± 13.9 |
62.3 ± 14.8 |
64.8 ± 13.9 |
0.60 |
| TLC % predicted |
73.0 ± 18.3 |
79.0 ± 18.6 |
74.0 ± 18.2 |
0.47 |
| DLCO % predicted |
58.0 ± 17.4 |
49.4 ± 21.7 |
56.5 ± 18.2 |
0.27 |
| HRCT Pattern (n, %) |
|
|
|
0.81 |
| Alternative |
34 (85.0%) |
13 (92.9%) |
47 (87.0%) |
|
| Probable UIP |
3 (7.5%) |
0 (0.0%) |
3 (5.6%) |
|
| Indeterminant for UIP |
3 (7.5%) |
1 (7.1%) |
4 (7.4%) |
|
As previously reported [
20], there were no statistically significant differences in adverse events between hospitalized and outpatients, including the incidence of pneumothorax (9%,
n = 2
vs. 5%,
n = 3), tube thoracostomy placement (5%,
n = 1
vs. 2%,
n = 1), grade 2 bleeding (defined as suctioning for more than 1 min or instillation of vasoconstricting agents) (9%,
n = 2
vs. 0%,
n = 0), escalation in level of care (5%,
n = 1
vs. 0%,
n = 0), 30-day mortality (9%,
n = 2
vs. 2%,
n = 1), and 60-day mortality (9%,
n = 2
vs. 4%,
n = 2) (
p > 0.05 for all). No deaths were attributed directly to the procedure.
A final MDD diagnosis was obtained in 96% (
n = 52) of patients (inpatient 100%,
n = 14
vs. outpatients 95%,
n = 38) (
p = 1) (
). The most common overall diagnosis was chronic hypersensitivity pneumonitis (31.5%,
n = 17), which was primarily driven by the outpatient group (40.0%,
n = 16), followed by connective tissue disease-related interstitial lung disease (11.1%,
n = 6), NSIP (11.1%,
n = 6), and organizing pneumonia (9.3%,
n = 5). Two (3.7%) patients (both outpatients) were determined to have unclassifiable ILD and did not receive a definitive diagnosis.
.
Multidisciplinary Conference Diagnoses.
|
Outpatient
N = 40 |
Inpatient
N = 14 |
Total
N = 54 |
p Value |
| MDD Diagnosis Received (N, %) |
38 (95.0%) |
14 (100%) |
52 (96.3%) |
1 |
| Specific MDD Diagnoses (N, %) |
|
|
|
|
| Chronic HP |
16 (40.0%) |
1 (7.1%) |
17 (31.5%) |
|
| CTD-ILD |
5 (12.5%) |
1 (7.1%) |
6 (11.1%) |
|
| NSIP |
4 (10.0%) |
2 (14.3%) |
6 (11.1%) |
|
| Organizing Pneumonia |
1 (2.5%) |
4 (28.6%) |
5 (9.3%) |
|
| Drug Induced Pneumonitis |
2 (5.0%) |
2 (14.3%) |
4 (7.4%) |
|
| Granulomatous Pneumonitis |
4 (10.0%) |
0 (0.0%) |
4 (7.4%) |
|
| Unclassifiable ILD |
2 (5.0%) |
0 (0.0%) |
2 (3.7%) |
|
| CFILD |
1 (2.5%) |
1 (7.1%) |
2 (3.7%) |
|
| IPF |
2 (5.0%) |
0 (0.0%) |
2 (3.7%) |
|
| 1 Other |
3 (7.5%) |
3 (21.4%) |
6 (11.1%) |
|
The inpatient group had significantly shorter time intervals from initial IP consult to biopsy (2.5 ± 4.4 days
vs. 15.5 ± 16.1 days,
p < 0.001), from biopsy to medical therapy change (10.3 ± 7.9 days
vs. 34.6 ± 37.0 days,
p < 0.001), and from initial IP consult to medical therapy change (12.8 ± 10.8 days
vs. 50.1 ± 38.5 days,
p < 0.001) (
). Inpatients also had less variability in time intervals compared to outpatients, as reflected by their corresponding smaller standard deviations, narrower interquartile ranges, and smaller overall ranges.
.
Time Intervals Between Events.
|
Outpatient |
Inpatient |
Total |
p Value |
Consult to Biopsy Days
(mean ± SD) |
15.5 ± 16.1 |
2.5 ± 4.4 |
12.1 ± 15.1 |
p < 0.001 |
Consult to Biopsy Days
(IQR, Range) |
20.5, 0–71 |
3.0, 0–17 |
18.5, 0–71 |
|
Biopsy to Treatment Days
(mean ± SD) |
34.6 ± 37.0 |
10.3 ± 7.9 |
28.3 ± 33.7 |
p < 0.001 |
Biopsy to Treatment Days
(IQR, Range)
|
28.0, 6–189 |
13.3, 1–24 |
23.3, 1–189 |
|
Consult to Treatment Days
(mean ± SD) |
50.1 ± 38.5 |
12.8 ± 10.8 |
40.4 ± 37.3 |
p < 0.001 |
Consult to Treatment Days
(IQR, Range)
|
37.5, 6–196 |
10.8, 1–41 |
41.0, 1–196 |
|
Patients in whom treatment was directly impacted by TBLC results were evaluated for differences in the types of medical therapy changes, defined as medication initiation of immunosuppression, anti-fibrotic, or other medications or medication changes, including adjustment or cessation (
). There were no significant differences in medical therapy changes between the groups (
p = 0.45). Initiation of immunosuppression was most common (70%,
n = 38) and was similarly enacted between inpatients (64%,
n = 9) and outpatients (72.5%,
n = 29).
.
Medication Changes.
|
Outpatient N = 40 |
Inpatient
N = 14 |
Total
N = 54 |
p Value |
| Treatment Medications (N, %) |
|
|
|
0.45 |
| Immunosuppression |
29 (72.5%) |
9 (64.3%) |
38 (70.4%) |
|
| Prednisone |
14 (35.0%) |
8 (57.1%) |
22 (40.7%) |
|
| Mycophenolate |
7 (17.5%) |
1 (7.1%) |
8 (14.8%) |
|
| Mycophenolate + Prednisone |
3 (7.5%) |
0 (0.0%) |
3 (5.6%) |
|
| Methotrexate |
1 (2.5%) |
0 (0.0%) |
1 (1.9%) |
|
| Azathioprine |
1 (2.5%) |
0 (0.0%) |
1 (1.9%) |
|
| Azithromycin |
3 (7.5%) |
0 (0.0%) |
3 (5.6%) |
|
| Anti-fibrotic |
4 (10%) |
1 (7.1%) |
5 (9.3%) |
|
| Nintedanib |
3 (7.5%) |
1 (7%) |
4 (7.4%) |
|
| Pirfenidone |
1 (2.5%) |
0 (0.0%) |
1 (1.9%) |
|
| Other |
6 (15.0%) |
2 (14.3%) |
8 (14.8%) |
|
| Antibiotic |
4 1 (10.0%) |
1 2 (7.1%) |
5 (9.3%) |
|
| Rituximab |
1 (2.5%) |
0 (0.0%) |
1 (1.9%) |
|
| Ruxolitinib |
0 (0.0%) |
1 (7.1%) |
1 (1.9%) |
|
| Inhaled therapy |
1 3 (2.5%) |
0 (0.0%) |
1 (1.9%) |
|
| Medication Change |
1 4 (2.5%) |
2 5 (14.3%) |
3 (5.6%) |
|
4. Discussion
Patients with ILD often wait a prolonged time between the initial presentation, the establishment of a diagnosis, and the initiation of medical therapy [
1,
2]. Therefore, it is important to identify opportunities to improve efficiency in the diagnostic process. With the development of more data supporting the efficacy of TBLC for diagnosing ILD, acutely ill, hospitalized inpatients with ILD may benefit from an expedited diagnosis to guide treatment. Our initial results evaluating wait times for newly identified ILD inpatients and outpatients show that inpatients have a significantly decreased wait time from initial consultation to lung biopsy and to changes in medical therapy.
A potential concern when performing TBLC on inpatients is the severity of the illness that warranted their hospitalization. SLB has been shown to be potentially prohibitive for hospitalized patients due to higher mortality compared to elective, ambulatory patients [
16,
17,
18]. In contrast, initial studies on inpatients undergoing TBLC have shown that while they are more acutely ill as measured by ASA score, supplemental oxygen need, and comorbidities, complication rates are not higher compared to outpatients for pneumothorax, bleeding, need for a higher level of care, or mortality [
19,
20]. While the size of these studies is limited (
n = 17 inpatients [
19] and
n = 22 inpatients [
20]), these findings are supported by other studies comparing inpatients and outpatients for other bronchoscopic procedures, such as endobronchial ultrasound-guided transbronchial needle aspiration [
21] and flexible bronchoscopy with bronchoalveolar lavage on intubated patients [
22]. Although the indications for these various procedures and patient populations are certainly different, the safety profiles further support performing bronchoscopic procedures on inpatients. Thus, consideration of inpatient TBLC to facilitate a diagnosis of ILD and treatment initiation appears reasonable.
HRCT is a crucial component in the diagnostic algorithm for ILD [
23]. The positive predictive value of an HRCT diagnosis of UIP is at least 90% in studies looking at patients with biopsy-proven diagnoses [
6]. While overt radiographic abnormalities are regularly recognized, subtle imaging changes are more challenging to identify, demonstrating the complexity of HRCT interpretation [
24]. This potential for conflicting data between imaging and biopsy results presents another concern regarding inpatient TBLC. While there are limited data looking at ILD resolution on serial imaging, it is possible that hospitalized patients with newly identified ILD could have short interval follow up imaging that refutes the possibility of ILD similar to incidentally found pulmonary parenchymal nodules [
25] and airway nodules of the tracheobronchial tree [
26]. In our study population, ten patients (six outpatients, four inpatients,
) received an alternative diagnosis despite the presence of what appeared to be ILD on imaging, further reflecting this potential discordance between radiographic and histopathologic diagnoses. However, we were able to establish an alternative diagnosis for these patients that guided their treatment, supporting the benefit of the biopsy procedure in their overall management. To mitigate the risk of an unnecessary procedure, it will be imperative to ensure that all alternative explanations for an ILD pattern on imaging, such as infection, interstitial edema, or malignancy, amongst others, are thoroughly examined before proceeding. Optimizing this process will be an area of future discussion.
ILD is uncommon in younger patients, with the mean age at diagnosis for IPF being 68 [
27]. Unfortunately, older age at diagnosis is associated with worse outcomes for patients with IPF [
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28], other progressive fibrosing interstitial lung diseases [
29], and rheumatoid arthritis associated with ILD [
5]. Because establishing a diagnosis of ILD is often delayed and exposes patients to unneeded procedures [
1,
2], years may pass before starting a treatment plan [
1,
2], potentially missing the opportunity to intervene earlier in the disease course before inflammation evolves into fibrosis. Interestingly, in our study, inpatients (59.4 ± 9.5 years) presented at a significantly earlier age than outpatients (65.9 ± 11.3 years;
p = 0.02,
) for TBLC. Although we are limited by our small sample size, this finding potentially suggests that these patients may be able to take advantage of a diagnosis at a significantly earlier age than outpatients, further supporting the finding of significant delays that outpatients with ILD experience. It is possible that the worse outcomes associated with advancing age may reflect the negative impact of a prolonged delay from symptoms to diagnosis and treatment. Thus, improving the efficiency of the diagnostic process may have the potential to impact morbidity and mortality.
A portion of ILD patients will develop chronic, fibrosing, and progressive disease. While IPF is the exemplar of this process, non-IPF ILDs may also evolve into a progressive pulmonary fibrosis (PPF) phenotype, which is characterized by worsening symptoms, radiographic progression, and physiological progression over the past year [
10]. PPF leads to a decline in lung function, decreased quality of life, and early mortality [
30]. Unfortunately, prognosticating which patients will develop this phenotype is challenging [
31]. Because fibrosis is irreversible, treatment should be initiated as soon as a diagnosis is confirmed for IPF [
32,
33] and once evidence of PPF is confirmed based on established criteria [
10]. In our study, inpatients undergoing TBLC waited significantly less time from IP consultation to biopsy (2.5 ± 4.4 days
vs. 15.5 ± 16.1 days,
p < 0.001), from biopsy to treatment (10.3 ± 7.9 days
vs. 34.6 ± 37.0 days,
p < 0.001), and most importantly from initial IP consult to treatment initiation (12.8 ± 10.8 days
vs. 50.1 ± 38.5 days,
p < 0.001) (
) compared to outpatients. It is reasonable to hypothesize that these findings suggest a potential positive impact on patient outcomes if lung function and lung structure are preserved through a more expeditious and efficient diagnostic and management process. Longitudinal studies assessing this possibility will be an area of future research.
While TBLC may present an efficient means to obtain an ILD diagnosis and establish a treatment plan, the need to obtain prior insurance authorization for certain medications may prevent patients from receiving their prescribed therapy. Studies from multiple medical specialties have shown that when prior insurance authorization is required, the time between medical therapy prescription and initiation of therapy is delayed, often due to denials for prior insurance authorization [
34,
35,
36]. Delays in initiating medications may lead to worse outcomes, as seen in post-cardiac stent patients who are unable to obtain anti-platelet therapy in a timely manner [
34]. Efforts to combat this barrier include the utilization of a centralized pharmacy [
37] and identifying individuals or teams to champion the process [
38]. Further efforts to accelerate the prior insurance authorization process will be needed to ensure that once a diagnosis is established and medical therapy is prescribed, patients will be able to begin their treatment quickly.
Although not examined in this study, there may also be a role for TBLC in evaluating inpatients with known ILD admitted for an acute exacerbation or concern for disease progression. While guidelines recommend ruling out cardiac failure or volume overload as part of the diagnostic criteria for an acute exacerbation of IPF [
39] or other ILDs [
40], the role of bronchoscopy with bronchoalveolar lavage to evaluate for infection as the inciting event or TBLC to obtain histopathology in this evaluation requires additional investigation [
39]. In lung transplant patients undergoing both surveillance bronchoscopy and those suspected of experiencing acute cellular rejection, TBLC, compared to the gold standard conventional transbronchial forceps biopsy [
41], improved the diagnostic accuracy of acute cellular rejection and led to treatment changes with an acceptable safety profile [
42,
43]. Extrapolating from this population, it may be beneficial to understand if histopathology for ILD patients with a suspected acute exacerbation or progression shows a change from an inflammatory state that requires additional or alternative immunosuppression to a fibrotic state that would be better suited by treatment with anti-fibrotic therapy. The potential impact of the information gained by TBLC on altering treatment regimens will require formal studies in the future.
Our study has limitations. These include its design as a single center and retrospective analysis with a small sample size, thus potentially impacting the rate of complications seen in our groups. Additionally, patients were not able to be randomized between the two groups, given the nature of their presentation for evaluation. However, it is strengthened by its inclusive nature of all patients with new ILD from both the inpatient and outpatient environments and the ability to obtain complete data points on all patients. We were able to show that inpatients with a new diagnosis of ILD present at a younger age (
) and wait less time to initiate medical therapy and to obtain a treatment determining TBLC procedure (
) compared to outpatients.
Because patients with ILD experience significant delays in establishing a diagnosis and initiating treatment, efforts to improve this process are essential. TBLC is a guideline recommended option to obtain a tissue diagnosis for patients with ILD. Our study shows that inpatients undergoing TBLC have a significantly decreased wait time from initial consultation to biopsy and to medical therapy changes, including medication initiation, adjustment, or cessation. Accelerating this process has the potential to positively impact patients by preventing progressive lung loss due to prolonged wait times. Evaluating the clinical impact of using TBLC to expedite and ILD diagnosis will require future prospective, longitudinal studies.
Author Contributions
All authors were responsible for data collection and accuracy of data, analysis of results, finalization of the manuscript, and approval of the submitted article. C.C. and B.S.B. conceived and wrote the manuscript and take responsibility for the integrity of the work as a whole.
Ethics Statement
Approval was obtained from the institutional review board of the Medical College of Wisconsin PRO00036023, Date of Approval: 5 March 2020.
Informed Consent Statement
Patient consent was waived by the institutional review board due to the retrospective nature and minimal risk of this research study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.
Funding
This research received no external funding.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1.
Pritchard D, Adegunsoye A, Lafond E, Pugashetti JV, DiGeronimo R, Boctor N, et al. Diagnostic test interpretation and referral delay in patients with interstitial lung disease.
Respir. Res. 2019,
20, 253.
[Google Scholar]
2.
Cosgrove GP, Bianchi P, Danese S, Lederer DJ. Barriers to timely diagnosis of interstitial lung disease in the real world: the Intensity survey.
BMC Pulm. Med. 2018,
18, 9.
[Google Scholar]
3.
Collard HR, Tino G, Noble PW, Shreve MA, Michaels M, Carlson B, et al. Patient experiences with pulmonary fibrosis.
Respir. Med. 2007,
101, 1350–1354.
[Google Scholar]
4.
Lamas DJ, Kawut SM, Bagiella E, Philip N, Arcasoy SM, Lederer DJ. Delayed access and survival in idiopathic pulmonary fibrosis: a cohort study.
Am. J. Respir. Crit. Care Med. 2011,
184, 842–847.
[Google Scholar]
5.
Cano-Jiménez E, Vázquez Rodríguez T, Martín-Robles I, Castillo Villegas D, Juan García J, Bollo de Miguel E, et al. Diagnostic delay of associated interstitial lung disease increases mortality in rheumatoid arthritis.
Sci. Rep. 2021,
11, 9184.
[Google Scholar]
6.
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management.
Am. J. Respir. Crit. Care Med. 2011,
183, 788–824.
[Google Scholar]
7.
Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. Diagnosis of Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline.
Am. J. Respir. Crit. Care Med. 2018,
198, e44–e68.
[Google Scholar]
8.
Troy LK, Grainge C, Corte TJ, Williamson JP, Vallely MP, Cooper WA, et al. Diagnostic accuracy of transbronchial lung cryobiopsy for interstitial lung disease diagnosis (COLDICE): a prospective, comparative study.
Lancet. Respir. Med. 2020,
8, 171–181.
[Google Scholar]
9.
Kalverda KA, Ninaber MK, Wijmans L, von der Thüsen J, Jonkers RE, Daniels JM, et al. Transbronchial cryobiopsy followed by as-needed surgical lung biopsy versus immediate surgical lung biopsy for diagnosing interstitial lung disease (the COLD study): a randomised controlled trial.
Lancet. Respir. Med. 2024,
12, 513–522.
[Google Scholar]
10.
Raghu G, Remy-Jardin M, Richeldi L, Thomson CC, Inoue Y, Johkoh T, et al. Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline.
Am. J. Respir. Crit. Care Med. 2022,
205, e18–e47.
[Google Scholar]
11.
Ravaglia C, Bonifazi M, Wells AU, Tomassetti S, Gurioli C, Piciucchi S, et al. Safety and Diagnostic Yield of Transbronchial Lung Cryobiopsy in Diffuse Parenchymal Lung Diseases: A Comparative Study versus Video-Assisted Thoracoscopic Lung Biopsy and a Systematic Review of the Literature.
Respiration 2016,
91, 215–227.
[Google Scholar]
12.
Kheir F, Uribe Becerra JP, Bissell B, Ghazipura M, Herman D, Hon SM, et al. Transbronchial Lung Cryobiopsy in Patients with Interstitial Lung Disease: A Systematic Review.
Ann. Am. Thorac. Soc. 2022,
19, 1193–1202.
[Google Scholar]
13.
Sharp C, McCabe M, Adamali H, Medford AR. Use of transbronchial cryobiopsy in the diagnosis of interstitial lung disease—a systematic review and cost analysis.
Int. J. Med. 2017,
110, 207–214.
[Google Scholar]
14.
Hernández-González F, Lucena CM, Ramírez J, Sánchez M, Jimenez MJ, Xaubet A, et al. Cryobiopsy in the diagnosis of diffuse interstitial lung disease: yield and cost-effectiveness analysis.
Arch. Bronconeumol. 2015,
51, 261–267.
[Google Scholar]
15.
Ost DE, Ernst A, Lei X, Kovitz KL, Benzaquen S, Diaz-Mendoza J, et al. Diagnostic Yield and Complications of Bronchoscopy for Peripheral Lung Lesions. Results of the AQuIRE Registry.
Am. J. Respir. Crit. Care Med. 2016,
193, 68–77.
[Google Scholar]
16.
Kreider ME, Hansen-Flaschen J, Ahmad NN, Rossman MD, Kaiser LR, Kucharczuk JC, et al. Complications of video-assisted thoracoscopic lung biopsy in patients with interstitial lung disease.
Ann. Thorac. Surg. 2007,
83, 1140–1145.
[Google Scholar]
17.
Han Q, Luo Q, Xie JX, Wu LL, Liao LY, Zhang XX, et al. Diagnostic yield and postoperative mortality associated with surgical lung biopsy for evaluation of interstitial lung diseases: A systematic review and meta-analysis.
J. Thorac. Cardiovasc. Surg. 2015,
149, 1394–1401.
[Google Scholar]
18.
Hutchinson JP, Fogarty AW, McKeever TM, Hubbard RB. In-Hospital Mortality after Surgical Lung Biopsy for Interstitial Lung Disease in the United States. 2000 to 2011.
Am. J. Respir. Crit. Care Med. 2016,
193, 1161–1167.
[Google Scholar]
19.
Cooley J, Balestra R, Aragaki-Nakahodo AA, Stamper DN, Sriprasart T, Swank Z, et al. Safety of performing transbronchial lung cryobiopsy on hospitalized patients with interstitial lung disease.
Respir. Med. 2018,
140, 71–76.
[Google Scholar]
20.
Castellani C, Castellani H, Benn BS. Transbronchial Lung Cryobiopsy is Safe and Effective for Diagnosing Acutely Ill Hospitalized Patients with New Diffuse Parenchymal Lung Disease.
Lung 2022,
200, 153–159.
[Google Scholar]
21.
Eapen GA, Shah AM, Lei X, Jimenez CA, Morice RC, Yarmus L, et al. Complications, consequences, and practice patterns of endobronchial ultrasound-guided transbronchial needle aspiration: Results of the AQuIRE registry.
Chest 2013,
143, 1044–1053.
[Google Scholar]
22.
Steinberg KP, Mitchell DR, Maunder RJ, Milberg JA, Whitcomb ME, Hudson LD. Safety of bronchoalveolar lavage in patients with adult respiratory distress syndrome.
Am. Rev. Respir. Dis. 1993,
148, 556–561.
[Google Scholar]
23.
American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001.
Am. J. Respir. Crit. Care Med. 2002,
165, 277–304; Erratum in
Am. J. Respir. Crit. Care Med. 2002,
166, 426.
[Google Scholar]
24.
Nishino M, Itoh H, Hatabu H. A practical approach to high-resolution CT of diffuse lung disease.
Eur. J. Radiol. 2014,
83, 6–19.
[Google Scholar]
25.
Semaan RW, Lee HJ, Feller-Kopman D, Lerner AD, Mallow CM, Thiboutot J, et al. Same-Day Computed Tomographic Chest Imaging for Pulmonary Nodule Targeting with Electromagnetic Navigation Bronchoscopy May Decrease Unnecessary Procedures.
Ann. Am. Thorac. Soc. 2016,
13, 2223–2228.
[Google Scholar]
26.
Kim HJ, Kim DK, Kim YW, Lee YJ, Park JS, Cho YJ, et al. Outcome of incidentally detected airway nodules.
Eur. Respir. J. 2016,
47, 1510–1517.
[Google Scholar]
27.
Garcia CK. Idiopathic pulmonary fibrosis: update on genetic discoveries.
Proc. Am. Thorac. Soc. 2011,
8, 158–162.
[Google Scholar]
28.
Ley B, Collard HR, King TE, Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis.
Am. J. Respir. Crit. Care Med. 2011,
183, 431–440.
[Google Scholar]
29.
Brown KK, Inoue Y, Flaherty KR, Martinez FJ, Cottin V, Bonella F, et al. Predictors of mortality in subjects with progressive fibrosing interstitial lung diseases.
Respirology 2022,
27, 294–300.
[Google Scholar]
30.
Cottin V, Wollin L, Fischer A, Quaresma M, Stowasser S, Harari S. Fibrosing interstitial lung diseases: knowns and unknowns.
Eur. Respir. Rev. 2019,
28, 180100.
[Google Scholar]
31.
Kolb M, Vašáková M. The natural history of progressive fibrosing interstitial lung diseases.
Respir. Res. 2019,
20, 57.
[Google Scholar]
32.
Torrisi SE, Pavone M, Vancheri A, Vancheri C. When to start and when to stop antifibrotic therapies.
Eur. Respir. Rev. 2017,
26, 170053.
[Google Scholar]
33.
Maher TM, Strek ME. Antifibrotic therapy for idiopathic pulmonary fibrosis: time to treat.
Respir. Res. 2019,
20, 205.
[Google Scholar]
34.
Ackman ML, Graham MM, Hui C, Tsuyuki RT. Effect of a prior authorization process on antiplatelet therapy and outcomes in patients prescribed clopidogrel following coronary stenting.
Can. J. Cardiol. 2006,
22, 1205–1208.
[Google Scholar]
35.
Wallace ZS, Harkness T, Fu X, Stone JH, Choi HK, Walensky RP. Treatment Delays Associated With Prior Authorization for Infusible Medications: A Cohort Study.
Arthritis. Care. Res. 2020,
72, 1543–1549.
[Google Scholar]
36.
Jew OS, Okawa J, Barbieri JS, McCaffrey J, Hayward E, Werth VP. Evaluating the effect of prior authorizations in patients with complex dermatologic conditions.
J. Am. Acad. Dermatol. 2020,
83, 1674–1680.
[Google Scholar]
37.
Popatia S, Flood KS, Golbari NM, Patel PV, Olbricht SM, Kimball AB, et al. Examining the prior authorization process, patient outcomes, and the impact of a pharmacy intervention: A single-center review.
J. Am. Acad. Dermatol. 2019,
81, 1308–1318.
[Google Scholar]
38.
Bhat S, Zahorian T, Robert R, Farraye FA. Advocating for Patients With Inflammatory Bowel Disease: How to Navigate the Prior Authorization Process.
Inflamm. Bowel. Dis. 2019,
25, 1621–1628.
[Google Scholar]
39.
Collard HR, Ryerson CJ, Corte TJ, Jenkins G, Kondoh Y, Lederer DJ, et al. Acute Exacerbation of Idiopathic Pulmonary Fibrosis. An International Working Group Report.
Am. J. Respir. Crit. Care Med. 2016,
194, 265–275.
[Google Scholar]
40.
Kolb M, Bondue B, Pesci A, Miyazaki Y, Song JW, Bhatt NY, et al. Acute exacerbations of progressive-fibrosing interstitial lung diseases.
Eur. Respir. Rev. 2018,
27, 180071.
[Google Scholar]
41.
Stewart S, Fishbein MC, Snell GI, Berry GJ, Boehler A, Burke MM, et al. Revision of the 1996 working formulation for the standardization of nomenclature in the diagnosis of lung rejection.
J. Heart. Lung. Transplant. 2007,
26, 1229–1242.
[Google Scholar]
42.
Steinack C, Gaspert A, Rüschoff J, Gautschi F, Hage R, Schuurmans M, et al. Transbronchial Cryobiopsy Compared to Forceps Biopsy for Diagnosis of Acute Cellular Rejection in Lung Transplant Recipients.
J. Heart. Lung. Trans. 2021,
40, S384–S385.
[Google Scholar]
43.
Steinack C, Gaspert A, Gautschi F, Hage R, Vrugt B, Soltermann A, et al. Transbronchial Cryobiopsy Compared to Forceps Biopsy for Diagnosis of Acute Cellular Rejection in Lung Transplants: Analysis of 63 Consecutive Procedures.
Life 2022,
12, 898.
[Google Scholar]