1. Introduction
Heart failure (HF) is a leading cause of hospitalization, with an increasing burden on healthcare systems [
1,
2]. Effective treatment relies on early detection and managing cardiac congestion. N-terminal pro–B-type natriuretic peptide (NT-proBNP) is a well-established biomarker for HF severity [
3,
4], but non-invasive alternatives are needed.
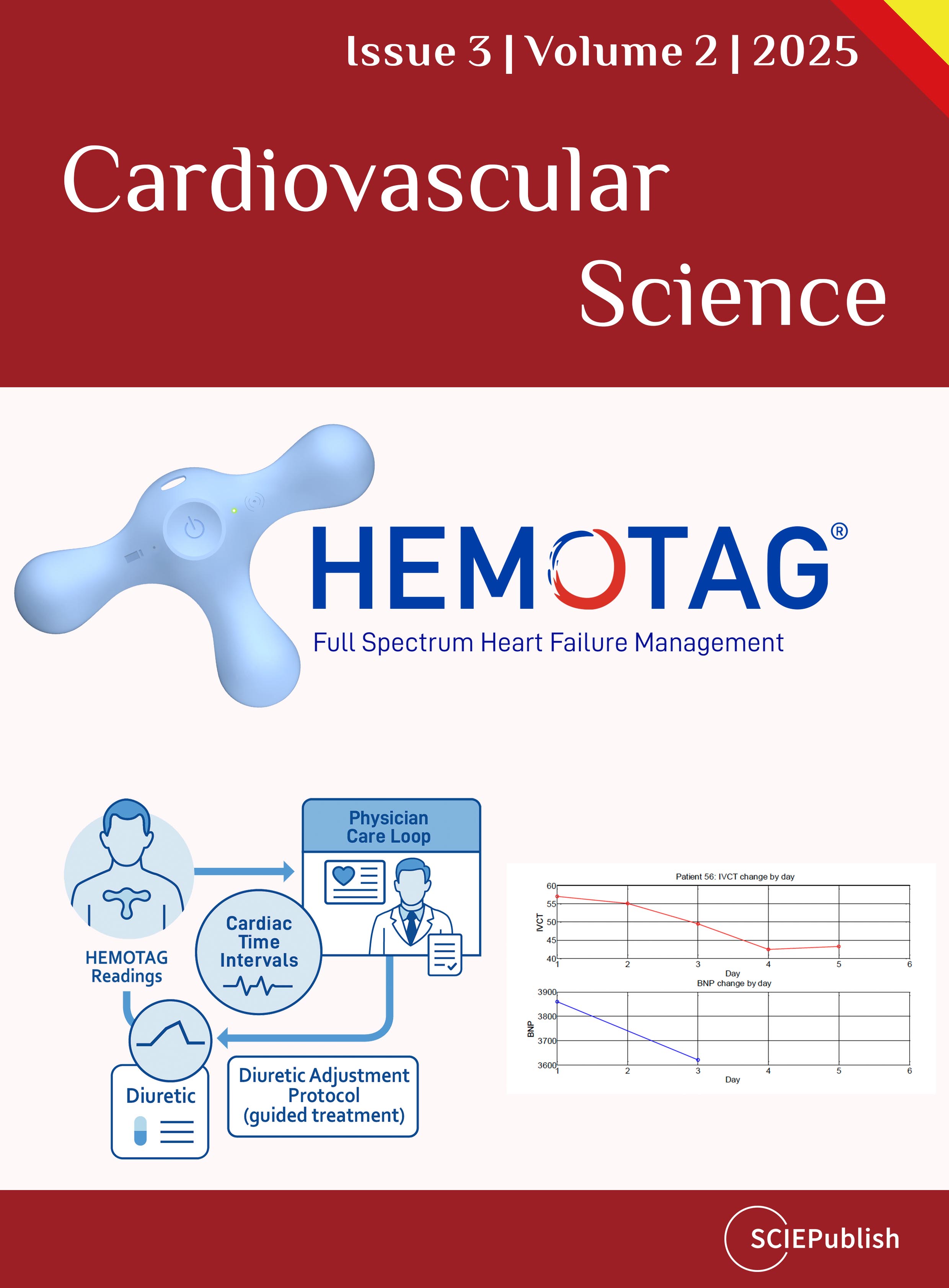
The HEMOTAG is a wearable, non-invasive device capable of capturing cardiac time intervals (CTIs), including isovolumetric contraction time (IVCT), which may correlate with HF status [
5,
6]. An increase in cardiac time intervals (CTIs) has been associated with early and accurate identification of acutely decompensated heart failure (ADHF). It is likely able to provide proactive and actionable guidance in tailoring therapy. Limited data are currently available regarding the feasibility of using the HEMOTAG device in clinical practice. This study aims to evaluate the association between CTI’s as measured by the HEMOTAG device compared with NT-proBNP levels, and daily evaluation of CTIs can guide treatment for patients with ADHF to improve short-term outcomes.
2. Materials and Methods
The HATS OFF (Hemotag AssessmenT for Short-term Outcomes oF heart Failure) Phase I study evaluates the clinical utility of HEMOTAG-derived CTIs in detecting and managing HF decompensation in patients hospitalized with ADHF. This prospective, unblinded, single-center, non-randomized study enrolled 105 patients hospitalized with ADHF (experimental arm) and other acute medical conditions not heart failure related (control arm) over a 4-month period. The aim of this study was to assess the relationship between daily IVCTs by the HEMOTAG device and the clinical progression of ADHF. An isovolumetric contraction time (IVCT) ≥ 40 ms was used as a marker of elevated CTIs as previously validated.
2.1. Study Design
HATS-OFF (Hemotag AssessmenT for Short-term Outcomes oF heart Failure) is a prospective, unblinded, single-center, non-randomized observational study designed to evaluate the clinical utility of the HEMOTAG in patients with acutely decompensated heart failure (ADHF). The study assessed the relationship between HEMOTAG-derived hemodynamic parameters and established clinical markers of heart failure. Institutional review board approval was obtained prior to study initiation.
2.2. Study Population
Patients were initially identified using ICD-10 code I50.9 in the emergency department or on the first day of hospitalization, and patient eligibility was further assessed based on the study’s inclusion and exclusion criteria. Eligible participants provided written informed consent before study enrollment. ADHF was determined based on the hospital admission presenting with symptoms, clinical signs of heart failure, and the need for urgent intravenous diuretics.
2.3. Intervention and Data Collection
All enrolled patients underwent non-invasive HEMOTAG measurements daily for up to seven days or until hospital discharge, whichever occurred first. Each recording was performed using a HEMOTAG wireless sensor. The data were transmitted in real-time to a secure mobile application and cloud-based dashboard. An isovolumetric contraction time (IVCT) ≥ 40 ms was used as a marker of elevated CTIs. Additional clinical data, including baseline demographics, laboratory values (NT-ProBNP levels on Days 1 and 3), length of hospital stay, and readmission rates at 30 and 90 days, were extracted from electronic medical records (EMR) and stored in a de-identified research database.
2.4. Endpoints
2.4.1. Primary Endpoint
To assess the association between HEMOTAG data and changes in NT-proBNP from baseline to day 3 of hospitalization.
2.4.2. Secondary Endpoints
Success in getting daily HEMOTAG measurements of acceptable quality and technical fidelity on recruited patients.
2.5. Safety and Ethical Considerations
The HEMOTAG system is classified as a non-significant risk (NSR) device by the Food and Drug Administration (FDA) with minimal potential harm to patients. The study involved no invasive procedures, and the risks associated with electrodes were limited to minor skin irritation or discomfort. Confidentiality was maintained through secure, de-identified data storage in a locked research facility.
2.6. Statistical Analysis
Descriptive statistics were used to summarize baseline characteristics. The relationship between HEMOTAG measurements and NT-ProBNP changes was assessed using correlation coefficients and confusion matrix analysis. Longitudinal changes in HEMOTAG-derived parameters were analyzed using paired t-tests. Readmission rates were evaluated against HEMOTAG data obtained close to discharge.
2.7. Study Criteria
2.7.1. Inclusion Criteria
- 1.
-
Age greater than or equal to 22 years old.
- 2.
-
An index hospital admission for ADHF based on presenting with symptoms, clinical signs of heart failure, and the need for urgent intravenous diuretics.
2.7.2. Exclusion Criteria
- 1.
-
Exclude enrollment by consent of a legally authorized representative.
- 2.
-
Terminal condition with a life expectancy of less than 90 days.
A control cohort of hospitalized patients without a diagnosis of ADHF was utilized as a second subset within the study.
2.8. Device Description
The HEMOTAG system consists of a sensor that is placed on the chest wall and can be used to capture 30-s measurements of electrical and heart vibrations in patients (). The system consists of the HEMOTAG sensor, the HEMOTAG mobile application, and the HEMOTAG cloud, which together provide the end-to-end operation. Data captured by the sensor is securely transmitted via an encrypted wireless connection to the HEMOTAG Mobile App. Data is then sent through an encrypted cellular or Wi-Fi connection to the HEMOTAG central computing software, where it is temporarily stored for report generation (). The HEMOTAG Report, which provides insights into cardiac function, is then made available to the Investigator as a PDF file.
. (<b>a</b>) HEMOTAG wireless sensor, (<b>b</b>) HEMOTAG Kit (Device and Mobile Application).
. HEMOTAG Data collection process.
3. Theory
The Application of Cardiac Time Intervals (CTIs) to Estimate Absolute Biomarkers
CTIs are defined by the opening and closing of the aortic and mitral valve with respect to the start of the QRS complex: Aortic Valve Opening (AVO), Aortic Valve Closing (AVC), Mitral Valve Closing (MVC), and Mitral Valve Opening (MVO).
Isovolumic contraction time (IVCT = Closing of the Mitral valve to the opening of the Aortic valve = AVO − MVC).
In large prospective studies, cardiac time intervals have been suggested and investigated as potential markers of hemodynamics for many years [
7,
8], as they are indicative of myocardial structure and function, containing physiological information about hemodynamics, namely, pulmonary artery pressures and both left ventricular systolic and left ventricular diastolic function. Multiple large studies have validated the relationship and accuracy between the CTIs and systolic and diastolic function assessed using left ventricular ejection fraction, global longitudinal strain, and global longitudinal strain rate [
9]. The prognostic value of CTIs has previously been shown in various populations [
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21].
4. Results
4.1. Primary Endpoint 1—Results
ADHF was diagnosed based on hospital admission, presenting with symptoms, clinical signs, and the need for urgent intravenous diuretics. An isovolumetric contraction time (IVCT) of 40 ms was used as a marker of elevated CTIs. Eight patients were eliminated from data analysis due to unusable electrocardiogram (EKG) data or no available NT-proBNP levels. Of 97 patients who met the criteria, 44% were female, 13% were African American (Race), and 27% Hispanics (Ethnicity). The mean age and mean BMI were 63 ± 17 years and 30.5 ± 9.2 kg/m
2, respectively (). The disease table for both groups is also shown ().
The mean initial NT-proBNP for the experimental arm (47 patients) was 8319 pg/mL, and the mean IVCT was 53 ms. For the control arm (50 patients), the mean initial NT-proBNP was 362 pg/mL, while the mean IVCT was 32 ms. ().
As demonstrated in , an IVCT ≥ 40 ms showed a strong sensitivity and specificity to detect ADHF (NT-proBNP ≥ 1800 pg/mL). shows the scatter plot of IVCT vs NT-proBNP.
.
Patient Demographics.
| Measure |
N |
Mean |
Standard Deviation |
Median |
Min |
Max |
| Age (years) |
97 |
62.99 |
16.89 |
64 |
22 |
91 |
| Weight (kg) |
97 |
90.27 |
33.16 |
81.50 |
43 |
259 |
| BP systolic |
97 |
128.92 |
41.39 |
128 |
84 |
182 |
| BP diastolic |
97 |
73.16 |
9.95 |
73 |
53 |
98 |
| Height (cm) |
97 |
170.66 |
11.14 |
170 |
149 |
205 |
| BMI |
97 |
30.54 |
9.24 |
28.71 |
16.80 |
69.53 |
.
Clinical Characteristics and Cardiac Comorbidities.
| Disease States |
Number of Patients Experimental |
Number of Patients Control |
| 1. Fluid-management Problems |
43 |
5 |
| 2. Heart Failure (HF): |
43 |
9 |
| 2.1. Systolic HF |
18 |
6 |
| 2.2. Diastolic HF |
22 |
3 |
| 2.3. Systolic and Diastolic HF |
3 |
0 |
| 3. Coronary Artery Disease (CAD) |
25 |
12 |
| 4. Hypertension (HTN) |
43 |
34 |
| 5. Pulmonary hypertension (PHTN) |
14 |
0 |
| 6. Diabetes: |
26 |
15 |
| 6.1. Type I |
0 |
4 |
| 6.2. Type II |
26 |
11 |
| 7. Lung Disease |
11 |
5 |
| 8. Mitral Valve Disease: |
|
|
| 8.1. Mitral Regurgitation |
14 |
5 |
| 8.1.1. Mild |
6 |
4 |
| 8.1.2. Moderate |
6 |
1 |
| 8.1.3. Severe |
2 |
0 |
| 9. Aortic Valve Disease: |
|
|
| 9.1. Aortic Regurgitation |
3 |
3 |
| 9.1.1. Mild |
1 |
3 |
| 9.1.2. Moderate |
1 |
0 |
| 9.1.3. Severe |
1 |
0 |
| 9.2. Aortic Stenosis |
3 |
2 |
| 9.2.1. Mild |
1 |
1 |
| 9.2.2. Moderate |
2 |
1 |
| 9.2.3. Severe |
0 |
0 |
| 10. Tricuspid Valve Disease: |
|
|
| 10.1. Tricuspid Regurgitation |
14 |
2 |
| 10.1.1. Mild |
7 |
2 |
| 10.1.2. Moderate |
4 |
0 |
| 10.1.3. Severe |
3 |
0 |
| 11. Cardiomyopathy |
44 |
12 |
| 12. Left Ventricular Hypertrophy (LVH) |
1 |
0 |
| 13. NYHA HF |
44 |
11 |
| 13.1. Class 1 |
1 |
6 |
| 13.2. Class 2 |
16 |
4 |
| 13.3. Class 3 |
23 |
1 |
| 13.4. Class 4 |
4 |
0 |
| 14. Sleep Apnea |
12 |
6 |
| 15. Angina |
18 |
10 |
| 16. Previous Myocardial Infraction |
24 |
5 |
| 17. Pacemaker |
7 |
2 |
| 18. ICD |
10 |
1 |
| 19. Undergone Chemotherapy |
2 |
0 |
| 20. VTE |
1 |
2 |
| 21. AFIB |
25 |
4 |
| 22. COPD |
10 |
6 |
| 23. CKD |
14 |
3 |
.
HEMOTAG efficacy to detect ADHF (NT-proBNP ≥ 1800 pg/mL).
| Statistical Measure |
Result |
| Sensitivity |
95 |
| Specificity |
84 |
| Negative Predictive value |
94 |
| Positive predictive value |
87 |
| The area under the curve |
0.92 |
| R |
0.58 |
. NT-ProBNP and IVCT distribution on experimental and control groups.
. Scatter plot of IVCT vs. NT-proBNP.
Additional analyses were performed in which NTproBNP and HEMOTAG recordings were recorded on the day following admission as well as at discharge. In this cohort, 17 patients met the eligibility criteria for the analysis (IVCT recording for a minimum of three days and NT-pro-BNP levels on the day of admission and the third day of hospitalization). Of the 17 patients who met the criteria for this analysis, 12 patients had ADHF (experimental arm) and 5 patients had an acute medical condition different than heart failure (control arm). IVCTs were recorded on admission and then daily (during hospitalization), while NT-pro-BNP was collected on admission and the 3rd day of hospitalization.
For patients with ADHF, the initial NT-pro-BNP decreased from a mean of 5515 ± 2766 pg/mL to a mean of 3801 ± 3066 pg/mL
vs. in the control arm NT-pro-BNP went from a mean of 130 ± 72 pg/mL to a mean of 149 ± 71 pg/mL. The HEMOTAG recording device was used to track daily IVCTs in all patients. For ADHF patients, the mean IVCT went from 59 ± 10 ms (first day of hospitalization) to 49 ± 9 ms (final day of hospitalization). Conversely, the control arm did not have any significant changes in their daily IVCTs, as demonstrated by a mean of 38 ± 9 ms (first day of hospitalization) to a mean of 37 ± 3 ms (final day of hospitalization).
T-test suggests that the effect of the treatment the experimental group received while in the hospital affected the NT-ProBNP and IVCT values, while the untreated control group kept both values stable.
In the ADHF group: A
t-test was conducted to determine whether the initial NT-proBNP differed from the final NT-proBNP. The analysis produced a t-statistic of
t_Stat = 2.606,
p = 0.024, with a critical
t-value of
t_critical = 2.200 at α = 0.05 (two-tailed). Since |
t_Stat| >
t_critical, the null hypothesis was rejected, indicating a significant difference.
A
t-test was conducted to determine whether the initial IVCT differed from the final IVCT. The analysis produced a
t-statistic of
t_Stat = 2.853,
p = 0.015, with a critical
t-value of
t_critical = 2.200 at α = 0.05 (two-tailed). Since |
t_Stat| >
t_critical, the null hypothesis was rejected, indicating a significant difference.
In the control group: A
t-test was conducted to determine whether the initial NT-proBNP differed from the final NT-proBNP. The analysis produced a
t-statistic of
t_Stat = −1.631,
p = 0.178, with a critical
t-value of
t_critical = 2.776 at α = 0.05 (two-tailed). Since |
t_Stat| <
t_critical, the null hypothesis cannot be rejected, indicating no significant difference.
A
t-test was conducted to determine whether the initial IVCT differed from the final IVCT. The analysis produced a
t-statistic of
t_Stat = 0.264,
p = 0.804, with a critical
t-value of
t_critical = 2.776 at α = 0.05 (two-tailed). Since |
t_Stat| >
t_critical, the null hypothesis cannot be rejected, indicating no significant difference.
depicts the progression of IVCTs and NT-proBNP in a subject with ADHF (experimental arm).
. A progressive decrease in IVCT in a patient with ADHF as volume overload (congestion) decreases with daily diuretics.
A total of 178 HEMOTAG recordings were sent by the 97 patients evaluated. As the experimental group of the study consisted of patients with ADHF, it was expected that most of the data would be of fair or poor quality as vibrations and electrical signals are naturally fainter and noisier. The signal quality of the data received was evaluated following the Data Quality table shown in
.
The focus of this endpoint was to evaluate the success in getting daily HEMOTAG measurements of acceptable quality and technical fidelity on recruited patients and the impact of patient and medical staff training.
After two months of data collection, it was found that some of the sources of data quality degradation were due to incorrect use of the device. Following the re-training of medical staff, there was an improvement in data quality for both accelerometer and EKG/ECG signals, as can be seen in
and
.
. Accelerometer signal quality.
.
HEMOTAG Data Quality Table.
| QUALITY LEVEL |
HEMOTAG EKG/ECG |
HEMOTAG Heart Vibrational Signals |
| EXCELLENT |
QRS complex is clearly defined and has a very low noise level. |
The onset and offset of the signal are clearly identifiable, and the noise is very low compared to the main signal. |
| GOOD |
QRS complex defined, but some noise or wandering effect is present. |
The onset and offset of the signal are identifiable, but some noise is present in the system on some or all of the heartbeats. |
| FAIR |
QRS complex has a noticeable noise/wandering effect that may make it difficult to find the onset of the QRS complex at some heartbeats. |
The signal vibration level and the noise are comparable in amplitude, making it difficult to clearly define the onset and offset of the signal for some heartbeats. |
| ACCEPTABLE |
QRS complex has a noticeable noise/wandering effect that may make it difficult to find the onset of the QRS complex at most heartbeats. |
The signal vibration level and the noise are comparable in amplitude, making it difficult to clearly define the onset and offset of the signal for most heartbeats. A heart sound may be completely absent from the data. |
| UNACCEPTABLE |
EKG signal is unreadable. |
Accelerometer signal is unreadable. |
. EKG/ECG signal quality.
The change in HEMOTAG measurements and the direction of change in HEMOTAG measurements results are summarized under primary endpoint 2.
5. Discussion
Isovolumetric contraction time (IVCT) and N-terminal pro–B-type natriuretic peptide (NT-proBNP) are both critical markers in heart failure (HF) assessment. However, they provide insights from different physiological mechanisms. NT-proBNP serves as a biomarker of myocardial stress, released in response to ventricular wall tension and elevated cardiac filling pressures. Meanwhile, IVCT is a mechanical parameter that reflects ventricular contractility by measuring the time interval between mitral valve closure and aortic valve opening. This study demonstrated that daily IVCTs, as measured by the HEMOTAG recording device, can predict the progression and response to treatment (
i.e., volume status) of patients with ADHF.
The relationship between IVCT and NT-proBNP is complex yet interconnected. Prolonged IVCT has been observed in patients with both heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF) and is often associated with increased myocardial stiffness and delayed ventricular contraction [
22,
23]. As myocardial strain increases due to higher left ventricular filling pressures, NT-proBNP secretion also rises [
24]. This suggests that IVCT prolongation may be an indicator of myocardial stress [
5], providing a potential non-invasive alternative to NT-proBNP.
While existing literature has established independent associations between these two parameters, direct studies evaluating their correlation remain limited. Our study explores this relationship further, particularly in the context of non-invasive, real-time management.
The HEMOTAG provides a non-invasive method for measuring cardiac time intervals (CTIs), including IVCT, by integrating heart vibrations and electrocardiogram (EKG) data. This study aimed to assess the agreement between HEMOTAG-derived measurements and NT-proBNP levels, which could yield important clinical insights. By evaluating IVCT, HEMOTAG could detect subclinical myocardial stress. This would enable intervention and better prognostic stratification for heart failure patients. Additionally, IVCT measurement with HEMOTAG could be performed non-invasively at the bedside or remotely, unlike NT-proBNP, which requires laboratory testing. From a practical standpoint, this could reduce hospital readmissions for heart failure and hopefully would translate into cost savings.
Invasive devices, such as the CardioMEMS Heart Failure System [
24], have demonstrated that hemodynamic measurements allow more effective heart failure management, leading to fewer hospitalizations by identifying worsening cardiac dynamics prior to symptom onset. In view of the risk and cost of invasive devices and the growing number of patients needing convenient access to personalized disease management, there is a clear need for non-invasive methods that can accurately manage heart failure in the clinic and at home [
6]. HEMOTAG may be able to provide similar value in a non-invasive fashion.
Study limitations exist. Our study includes a relatively small population size and is a single-center study. Additionally, this study is observational, and all patients in the study arm already had a diagnosis of ADHF. Therefore, it is difficult to understand the efficacy of the HEMOTAG device in predicting the acute onset of decompensated heart failure. Although these limitations exist, the findings of this study help support additional research to further understand the utility of this device in predicting and preventing the onset of acutely decompensated heart failure.
The results of this study indicate a strong relationship between IVCT and NT-proBNP as there was a parallel decrease in HEMOTAG measured IVCT to NT-ProBNP levels as the ADHF patients were treated. This suggests that daily IVCTs by the HEMOTAG recording device could predict the progression and response to treatment
(i.e., volume status) of patients with ADHF.
6. Conclusions
This study demonstrates a significant relationship between the NT-proBNP biomarker and IVCT as measured by the non-invasive HEMOTAG device. It provides support for the use of the HEMOTAG device as a potential non-invasive tool in the identification of acutely decompensated heart failure. While NT-proBNP remains a standard biomarker, HEMOTAG’s ability to non-invasively manage a heart failure patient using IVCT may provide additional prognostic value. Future studies should aim to validate whether changes in IVCT correspond to changes in hemodynamics over time, paving the way for a more comprehensive approach to heart failure monitoring.
Acknowledgments
The authors gratefully acknowledge support from Aventusoft LLC for the HEMOTAG technology and funding from the National Heart, Lung, And Blood Institute under grant number R44HL145941.
Author Contributions
Conceptualization, R.C., F.R.T., J.E.P., D.U. and D.S.; Methodology, R.C., F.R.T., J.E.P., D.U. and D.S.; Software, R.C., F.R.T. and J.E.P.; Validation, R.C., F.R.T., J.E.P., D.U. and D.S.; Formal Analysis, D.U. and D.S.; Investigation, R.C., F.R.T., J.E.P., D.U. and D.S.; Resources, D.S.; Data Curation, D.U. and D.S.; Writing—Original Draft Preparation, R.C., F.R.T., J.E.P., D.U. and D.S.; Writing—Review & Editing, R.C., F.R.T., J.E.P., D.U. and D.S.; Visualization, R.C., F.R.T., J.E.P., D.U. and D.S.; Supervision, D.S.; Project Administration, D.S.; Funding Acquisition, D.S.
Ethics Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of University of Miami (Study Protocol: 20190420, date of approval: 6/30/2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data is protected as per the guidelines of SBIR data protection from for a period of not less than 20 years with the protection period beginning at the time of the Phase award (R44HL145941 - 06/01/2019).
Funding
This research was funded by the National Heart, Lung, And Blood Institute grant number R44HL145941.
Declaration of Competing Interest
The authors declare no conflict of interest.
References
1.
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association.
Circulation 2023,
147, e93–e621.
[Google Scholar]
2.
Heidenreich P, Bozkurt B, Aguilar D, Allen L, Byun J, Colvin M. 358 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American 359 College of Cardiology/American Heart Association Joint Committee on Clinical Practice 360 Guidelines.
Circulation 2022,
145, e895–e1032.
[Google Scholar]
3.
Teramoto K, Tay WT, Tromp J, Ouwerkerk W, Teng TK, Chandramouli C, et al. Longitudinal NT‐proBNP: Associations With Echocardiographic Changes and Outcomes in Heart Failure.
J. Am. Hear. Asso. 2024,
13, e032254.
[Google Scholar]
4.
Corteville DC, Bibbins-Domingo K, Wu AH, Ali S, Schiller NB, Whooley MA. N-terminal pro–B-type natriuretic peptide as a diagnostic test for ventricular dysfunction in patients with coronary disease: data from the heart and soul study.
Arch. Intern. Med. 2007,
167, 483–489.
[Google Scholar]
5.
Alhakak AS, Møgelvang R, Schnohr P, Modin D, Brainin P, Gislason G, et al. The cardiac isovolumetric contraction time is an independent predictor of incident heart failure in the general population.
Int. J. Card. 2020,
312, 81–86.
[Google Scholar]
6.
Boriani G, Da Costa A, Ricci RP, Strömberg A, Santini M, Landolina M, et al. The integration of devices and digital health tools in heart failure care: A European Heart Rhythm Association consensus document.
EP Europace 2022,
24, 29–44. doi:10.1093/europace/euab283.
[Google Scholar]
7.
Biering‐Sørensen T, Mogelvang R, Schnohr P, Jensen JS. Cardiac Time Intervals Measured by Tissue Doppler Imaging M-mode: Association With Hypertension, Left Ventricular Geometry, and Future Ischemic Cardiovascular Diseases.
J. Am. Heart Assoc. 2016,
5, e002687.
[Google Scholar]
8.
Biering-Sørensen T, Mogelvang R, Søgaard P, Pedersen SH, Galatius S, Jørgensen PG, et al. Prognostic Value of Cardiac Time Intervals by Tissue Doppler Imaging M-Mode in Patients With Acute STSegment- Elevation Myocardial Infarction Treated With Primary Percutaneous Coronary Intervention.
Circ. Cardiovasc. Imaging 2013,
6, 457–465.
[Google Scholar]
9.
Biering-Sørensen T, Jensen JS, Andersen HU, Rossing P, Jensen MT. Cardiac time intervals and the association with 2D-speckle-tracking, tissue Doppler and conventional echocardiography: The Thousand&1 Study.
Int. J. Cardiovasc. Imaging 2016,
32, 789–798.
[Google Scholar]
10.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography.
Eur. J. Echocardiogr. J. Work Group Echocardiogr. Eur. Soc. Cardiol. 2009,
10, 165–193.
[Google Scholar]
11.
Su HM, Lin TH, Voon WC, Lee KT, Chu CS, Yen HW, et al. Correlation of Tei index obtained from tissue Doppler echocardiography with invasive measurements of left ventricular performance.
Echocardiogr. Mt. Kisco. N. 2007,
24, 252–257.
[Google Scholar]
12.
Ärnlöv J, Ingelsson E, Risérus U, Andrén B, Lind L. Myocardial performance index, a Doppler-derived index of global left ventricular function, predicts congestive heart failure in elderly men.
Eur. Heart J. 2004,
25, 2220–2225.
[Google Scholar]
13.
Ärnlöv J, Lind L, Andrén B, Risérus U, Berglund L, Lithell H. A Doppler-derived index of combined left ventricular systolic and diastolic function is an independent predictor of cardiovascular mortality in elderly men.
Am. Heart. J. 2005,
149, 902–907.
[Google Scholar]
14.
Mishra RK, Kizer JR, Palmieri V, Roman MJ, Galloway JM, Fabsitz RR, et al. Utility of the myocardial performance index in a population with high prevalences of obesity, diabetes, and hypertension: the strong heart study.
Echocardiogry 2007,
24, 340–347.
[Google Scholar]
15.
Tei C, Dujardin KS, Hodge DO, Kyle RA, Tajik AJ, Seward JB. Doppler index combining systolic and diastolic myocardial performance: clinical value in cardiac amyloidosis.
J. Am. Coll. Cardiol. 1996,
28, 658–664 9.
[Google Scholar]
16.
Dujardin KS, Tei C, Yeo TC, Hodge DO, Rossi A, Seward JB. Prognostic value of a Doppler index combining systolic and diastolic performance in idiopathic-dilated cardiomyopathy.
Am. J. Cardiol. 1998,
82, 1071–1076.
[Google Scholar]
17.
Kim H, Yoon HJ, Park HS, Cho YK, Nam CW, Hur SH, et al. Usefulness of tissue Doppler imaging-myocardial performance index in the evaluation of diastolic dysfunction and heart failure with preserved ejection fraction.
Clin. Cardiol. 2011,
34, 494–499.
[Google Scholar]
18.
Correale M, Totaro A, Greco CA, Musaico F, De Rosa F, Ferraretti A, et al. Tissue Doppler time intervals predict the occurrence of rehospitalization in chronic heart failure: data from the daunia heart failure registry.
Echocardiogry 2012,
29, 906–913.
[Google Scholar]
19.
Sung SH, Yu WC, Cheng HM, Chang YP, Chen CH. Use of Acoustic Cardiography to Guide Outpatient Therapy of Patients with Acute Heart Failure Syndrome,
J. Am. College Cardiol. 2014,
63, A541.
[Google Scholar]
20.
Chao TF, Sung SH, Cheng HM, Yu WC, Wang KL, Huang CM, et al. Electromechanical Activation Time in the Prediction of Discharge Outcomes in Patients Hospitalized with Acute Heart Failure Syndrome,
Inter. Med. 2010,
49, 2031–2037.
[Google Scholar]
21.
Biering-Sørensen T, Mogelvang R, Jensen JS. Prognostic value of cardiac time intervals measured by tissue Doppler imaging M-mode in the general population.
Heart Br. Card. Soc. 2015,
101, 954–960.
[Google Scholar]
22.
Ghazal MN, Bouzas-Mosquera A, Edvardsen T. Cardiac time intervals by echocardiography: Current perspectives.
Int. J. Cardiol. 2020,
304, 135–141. doi:10.1016/j.ijcard.2019.12.036.
[Google Scholar]
23.
Ma C, Luo H, Fan L, Liu X, Gao C. Heart failure with preserved ejection fraction: an update on pathophysiology, diagnosis, treatment, and prognosis.
Braz. J. Medi. Biol. Res. 2020,
53, e9646.
[Google Scholar]
24.
CardioMEMS HF System Remote Pulmonary Pressure Monitor. Available online: https://www.cardiovascular.abbott/int/en/hcp/products/heart-failure/pulmonary-pressure-monitors/cardiomems/about.html (accessed on 1 April 2025).