Mental Health Impacts Associated with Exposure to Climate-Sensitive Hazards in Pacific Island Countries: A Scoping Review
Received: 09 July 2025 Revised: 08 September 2025 Accepted: 27 October 2025 Published: 05 November 2025
© 2025 The authors. This is an open access article under the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/).
1. Introduction
Pacific Island Countries (PICs) stand at the frontline of climate change impacts. PICs are increasingly experiencing a wide range of climate change-related extreme weather and climate events (extreme events), including cyclones, floods, droughts, changes in rainfall patterns, and sea level rise [1]. According to the Intergovernmental Panel on Climate Change (IPCC) Sixth Assessment Report (AR6), small island developing states (SIDS), including PICs, are exposed to risks of ecosystem loss, threats to lives and assets, economic decline, water insecurity, and increased displacement [2]. Moreover, these risks have aggravated health impacts in the region, including leptospirosis, typhoid, diarrhea, malaria, and psychological distress [1]. However, compared to other regions, evidence on the mental health impacts of extreme events and climate change remains limited in SIDS [2], including PICs.
Climate change affects mental health through immediate, direct, and long-term impacts, as well as indirect impacts [3]. Acute disasters, such as cyclones, reportedly increase Post Traumatic Stress Disorder (PTSD), acute stress disorder, sleep disorder, generalized anxiety disorder, suicidal ideation and depression [4,5], and rising temperatures are linked with self-harm and interpersonal violence [6]. These direct impacts can also generate long-term risks for mental health through indirect pathways such as conflict and violence, forced migration, loss of place attachment, community breakdown, worsened physical health, loss of livelihoods, disruption of health systems, and food and water insecurity [3]. Moreover, awareness of current and anticipated climate-related threats, coupled with perceptions of insufficient climate action, can evoke a wide range of psychological and emotional reactions [3]. These may include anxiety, worry, distress, anger, fear, grief, frustration, stress, denial, hopelessness, or helplessness, and have been described using terms such as eco-anxiety, climate distress, and solastalgia [3].
PICs have regional and cultural characteristics that serve as a distinct context for mental health impacts from extreme events and climate change. Most PICs consist of small islands with varying population densities, leading to significant geographical isolation, particularly in rural and outer island areas. This geographical isolation creates numerous challenges in delivering healthcare services. Moreover, in Pacific cultures, the land is viewed as a vital source of life, connecting people to their past, present, and future [7]. Given these perspectives and the collectivist cultural context, the loss of community could have a significant impact on people’s lives [8]. In Pacific Island contexts, the meanings of healing and illness are deeply rooted in a close relationship with nature; illnesses are believed to arise from a disruption in this connection [7]. These cultural characteristics may discourage individuals from sharing personal issues or seeking mental healthcare, which can contribute to underreporting and underestimation of mental health impacts.
PIC communities are experiencing major health impacts from climate change [1] that have the potential to aggravate mental health. Mental and substance use disorders have been identified as leading contributors to disability in the region, however, reports from several PICs indicate that approximately 90% of individuals with mental health conditions did not receive treatment [9]. Furthermore, a recent review of mental health impacts from climate change and sea level rise in the Pacific Islands identified only a few studies [10], highlighting a critical knowledge gap in understanding the cultural dimensions of mental health in the PIC context. In this study, the search strategy was limited to keywords related to climate change and sea level rise that may have excluded other climate-sensitive hazards. Additionally, the short- and long-term direct impacts and indirect impacts need to be considered by examining a range of climate-related events and extended hazard periods.
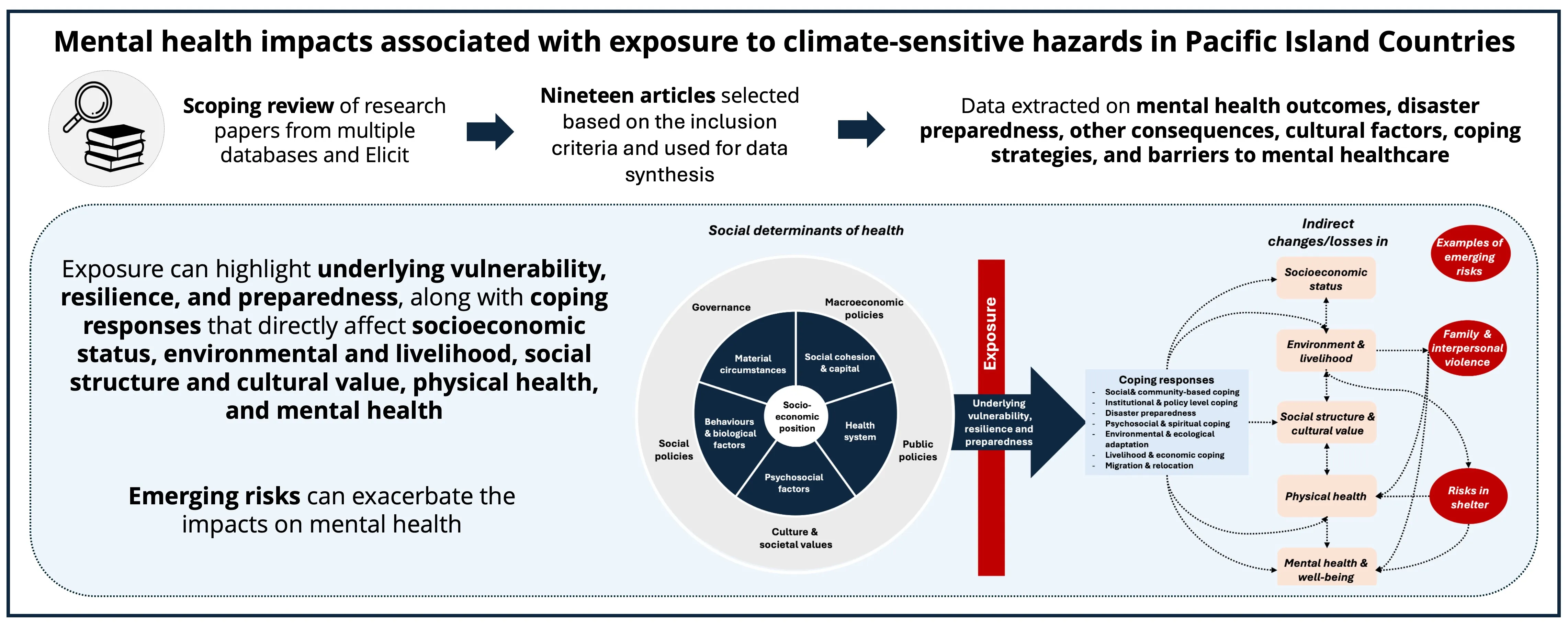
The magnitude and the pattern of mental health challenges will also depend on the social determinants of health. The structural determinants and socioeconomic positions contribute to differential exposure and vulnerability to climate-sensitive hazards [11]. Intermediary determinants, such as material circumstances, psychosocial circumstances, behavioral/biological factors, and health systems, along with broader socioeconomic and political contexts, can generate underlying vulnerabilities to these hazards [11]. Therefore, this scoping review aims to investigate the mental health impacts of diverse climate-sensitive hazards and their underlying factors, including disaster preparedness, cultural factors, coping strategies, and mental healthcare barriers in PICs.
2. Methods
A scoping review approach was selected to characterize studies on climate-related events and mental health impacts in PICs to provide an overview of the evidence [12]. This scoping review followed the Preferred Reporting Items for Systematic reviews and Meta-analyses extension for Scoping Reviews (PRISMA-ScR) statement guidance [13].
To identify original research studies related to mental health and climate change in the PICs, the following online databases were searched using PubMed and Web of Science databases in January 2025. All years were included for the literature search. For the PubMed search, both Medical Subject Headings (MeSH) terms and free-text terms were used. The search strategy included the name and region of PICs (“American Samoa” or “Cook Islands” or “Fiji” or “French Polynesia” or “Federated States of Micronesia” or “Guam” or “Kiribati” or “Mariana Islands” or “Nauru” or “New Caledonia” or “Niue” or “Palau” or “Papua New Guinea” or “Pitcairn Islands” or “Samoa” or “Solomon Islands” or “Tokelau” or “Tonga” or “Tuvalu” or “Vanuatu” or “Wallis and Futuna” or “Melanesia” or “Micronesia” or “Polynesia”) and one extreme events “climate change” or “droughts” or “floods” or “sea level rise” or “ocean acidification” or “cyclone” or “extreme weather” or “extreme heat” and mental health impacts for “mental health” was used. Each extreme event and the name and region of PICs were combined and searched separately with the term “mental health”. In addition, the broad term “Pacific Islands” or “SIDS” was used with “mental health”, “climate change”, and “indigenous people” for the initial search to include research on the indigenous population. The search term “climate change” enabled us to identify articles on temperature and precipitation in the context of a changing climate. Additional studies were identified using snowball methods that involved evaluating review articles from the initial search. Studies were selected for screening if they were relevant to our research scope and original articles.
We also used the artificial intelligence literature review tool, Elicit, to identify further studies. Elicit is an AI-based research assistant that provides concise summaries of research questions and supports the organization of relevant literature to identify and screen studies, as well as to extract key information [14]. The research question for Elicit was “Climate change and mental health impacts in Pacific Islands”, which was accessed in February 2025. In total, 500 papers were evaluated, with only 32 included, by automatically and manually adjusting the screening score threshold and screening description generated by Elicit. The score was based on criteria including article type, focus on climate change, dual focus on climate change and mental health, inclusion of indigenous knowledge, presence of a mental health component, target population, and study design (primary research or systematic review). The authors established these screening criteria to identify literature relevant to the research scope.
After all searches were done, the results were compiled, duplicates were removed, and the review proceeded as follows. One author (HM) independently conducted title/abstract and full-text screening using EndNote 20 and Covidence, and any ambiguities regarding which articles to include were discussed with the other two authors (J.J.H. and K.L.E.). Consensus was sought throughout the process. The inclusion criteria were (1) peer-reviewed journal articles; (2) reported climate change and mental health impacts in the PICs; and (3) full-text available and written in English. One short communication article was included in the scoping review because it includes the study design component and reporting of the original article [15].
After the final agreement was reached regarding inclusion, the data were extracted using the predefined Excel data extraction form, including the following columns: (1) country of focus; (2) climate exposure(s); (3) study design; (4) population of interest (main island/outer islands); (5) mental health outcomes; (6) disaster preparedness; (7) other consequences; (8) cultural factors; (9) coping strategies; and (10) mental healthcare barriers.
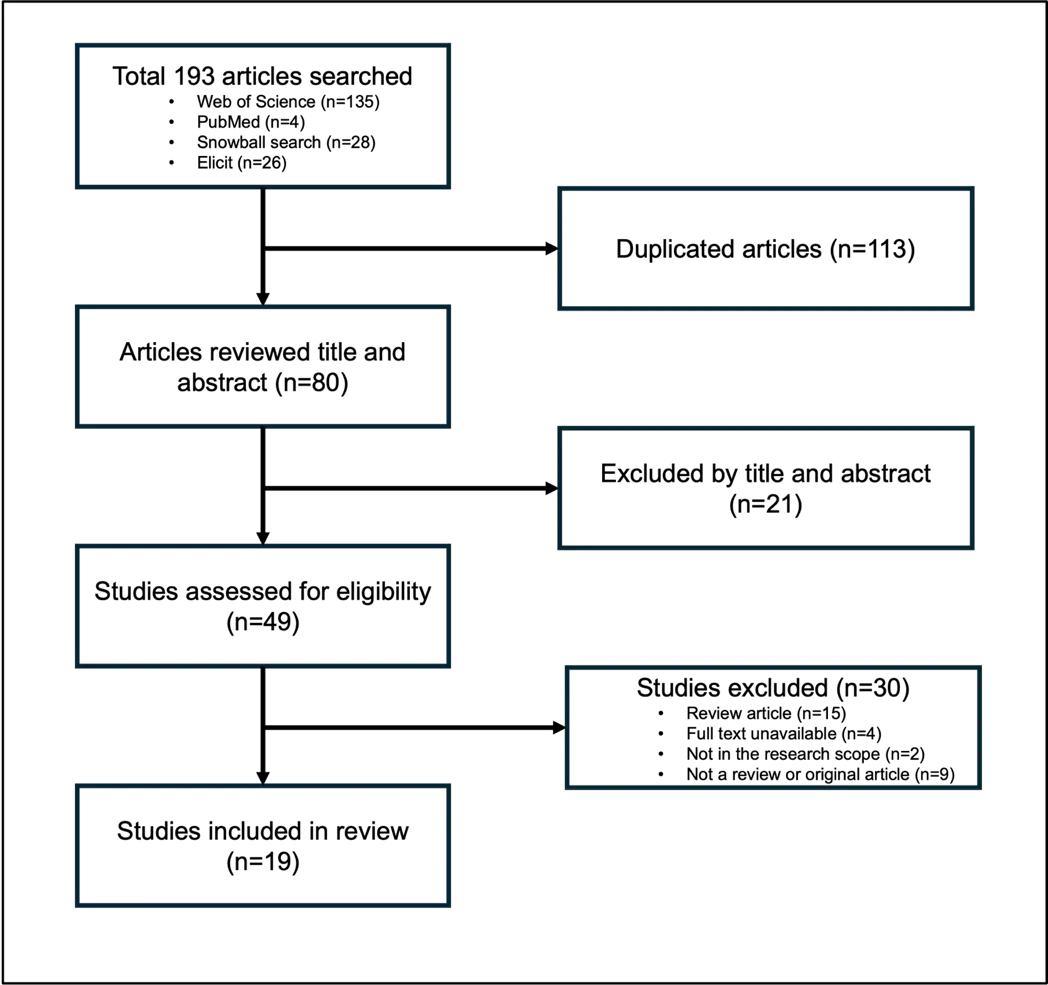
From the 193 articles retrieved at the initial screening, 49 articles were deemed relevant to the scoping review, of which 30 were then excluded for not meeting the criteria. This left 19 articles for the data synthesis (Figure 1).
3. Results
3.1. Overview of Results
Figure 1 details the results of the literature selection process that yielded 19 studies in the final sample. We identified 10 mixed-method studies, 8 qualitative studies, and one quantitative study. Among these studies, 15 were cross-sectional, while the others included a case study [16], a two-wave longitudinal study [15], a longitudinal case study [17], and a multi-year cross-sectional ethnographical study [18]. The exposure of interest in these papers included cyclones (n = 2), tsunamis (n = 1), storm/cyclones and droughts (n = 2), droughts (n = 1), sea level rise (n = 1), planned relocation (n = 1), and environmental concerns/changing climate (climate change) (n = 11) that examined general perceptions of climate change or environmental concerns. The publication years ranged from 2011 to 2024, reflecting the growing and recent focus on the mental health impacts of climate change-sensitive hazards. Sample sizes varied considerably across study designs, ranging from one to 71 participants in qualitative studies, 27 to 515 participants in mixed-methods studies, and up to 1365 participants in quantitative studies. The key findings from each study are summarized in Table 1, and detailed information is provided in Table S1.
Four articles were multi-national studies, and 15 articles were conducted in a single country, including Fiji (n = 4), Kiribati (n = 3), Tuvalu (n = 3), Cook Islands (n = 2), Solomon Islands (n = 1), Samoa (n = 1), Papua New Guinea (n = 1), Vanuatu (n = 1). Most of the specific study sites focused on the main island (n = 11), and four articles focused on both the main island and outer islands, while the last four articles did not mention specific study sites.
Among 10 mixed-method studies, four utilized existing survey instruments to assess mental health impacts. One study conducted in Papua New Guinea examined the effects of heavy storms and droughts on life satisfaction using a subjective well-being survey instrument [19]. A study in Vanuatu assessed damage and distress caused by a cyclone using a culturally adapted version of the Impact of Event Scale-Revised (IES-R) to measure subjective distress resulting from traumatic events [15]. In Tuvalu, a study investigating the psychological distress and associated impairment associated with local environmental impacts used a culturally adapted version of the Hopkins-Symptom Checklist (HSCL-25) to assess symptoms of anxiety and depression, along with a 4-point Likert scale to indicate distress levels for each local extreme event stressor to which participants had been exposed [20]. A study conducted across six PICs with college students assessed levels of environmental concern and attitudes using a five-item life satisfaction scale and an eight-item measure of social-psychological prosperity and flourishing [21].
3.2. Mental Health Outcomes
A wide range of mental health impacts were observed in relation to acute events, slow-onset events, and perception of climate change in PICs. In our scoping review, acute events referred to cyclones and tsunamis, while slow-onset events included droughts, sea level rise, and adaptation strategies such as planned relocation.
In PICs, acute events were reported to increase feelings of depression [22]. A case study in Samoa documented experiences of insomnia and anxiety after the tsunami events [16]. High levels of distress were observed in both pregnant and non-pregnant women [15], and another study reported heightened fear and stress after cyclones [23]. In the same study, one of the 11 participants described initial feelings of excitement and thrill during the first cyclone; however, this excitement faded after experiencing several subsequent and devastating cyclones [23].
Slow-onset events were also found to have strong, detrimental impacts on subjective well-being [19,24]. For example, individuals exposed to drought reported feelings of worry, sadness, anger, tiredness, and hopelessness [23,24]. Similarly, for sea level rise, concerns about daily life and family well-being were reported [25]. While planned relocation resulted in reduced anxiety related to flooding, coastal erosion, and saltwater intrusion, it also disrupted place attachment, negatively affecting mental health and well-being [17].
Studies exploring perceptions of climate change in PICs identified a wide range of emotional responses. Young adults in the region expressed strong environmental concerns, with low levels of environmental indifference [21]. Feelings of sadness, worry, and anxiety were reported in multiple countries [18,26,27,28]. However, some individuals in Kiribati remained unconcerned about climate change due to their strong faith in God [29]. Ecological grief, a sense of loss, a sense of injustice, and a lack of power led to hopelessness and anger [18,28,30,31]. Consecutive extreme events led to increased stress, anxiety, and fear within communities [31,32], ultimately negatively impacting mental health and well-being [20,27,33].
Table 1. Key mental health challenges in Pacific Island Countries are associated with extreme events, their consequences, or climate change.
|
Exposure |
Location of Exposure |
Study Design |
Outcome Measured |
Findings |
Population Characteristics |
Sample Size |
References |
|---|---|---|---|---|---|---|---|
|
Cyclone |
Tuvalu |
Qualitative method (cross-sectional study) |
How the Persons with Disabilities (PwDs) ability to prepare, their perceptions, and experiences with disasters have contributed to their resilience to disasters |
One participant mentioned that “I was there at the time Tropical Cyclone Pam hit my island, and I felt very depressed about the situation” |
|
31 PWDs (21 had a physical impairment, 2 were blind, and 8 were deaf or hard-of-hearing) |
[22] |
|
Tsunami |
Samoa |
Qualitative method (case study) |
Grief recovery processes in the Samoan cultural context (Examination of family history, cultural rituals, spiritual practices, and coping mechanisms) |
Grief resolution process
|
|
1 couple |
[16] |
|
Cyclone |
Vanuatu |
Quantitative method (two-wave longitudinal study) |
Distress (Bislama adaptation of IES-R) |
|
|
926 women in 2015 and 1365 in 2016 |
[15] |
|
Heavy storms and droughts |
Papua New Guinea |
Mixed-methods (cross-sectional study) |
Subjective well-being (SWB), personal experience of natural hazards, socioeconomic and demographic background |
|
|
515 participants (251 women and 264 men) |
[19] |
|
Drought and cyclone |
Cook Islands |
Qualitative method (cross-sectional study) |
Experiences and responses to extreme weather events (cyclones and droughts) |
Droughts
Cyclones
|
|
11 participants (4 women and 7 men) |
[23] |
|
Droughts |
Fiji |
Qualitative method (cross-sectional study) |
Local and national stakeholder perceptions of climate change loss and damage in Fiji |
|
|
20 sugar cane farmers and 28 key stakeholders |
[24] |
|
Sea level rise |
Solomon Islands |
Mixed-methods (cross-sectional study) |
Individual perceptions and responses to sea level rise, and community responses |
|
|
57 participants (31 men and 26 women) |
[25] |
|
Planned relocation |
Fiji |
Qualitative method (longitudinal case study) |
People’s perceptions of the health determinants and impacts of planned relocation |
Place attachment and well-being impacts
|
|
|
[17] |
|
Climate change |
Fiji, Vanuatu, Solomon Islands, Tuvalu, Samoa, and Tonga |
Mixed-methods (cross-sectional study) |
The signature strength survey, environmental concern, support for environmental actions and policies, environmental indifference, life satisfaction, flourishing |
|
|
|
[21] |
|
Climate change |
Fiji, Cyprus, New Zealand, and England |
Mixed-methods (cross-sectional study) |
Emotional responses in three domains (climate change and its effect on the respondents, livelihoods in the area, and its effect on the younger generation) |
|
|
68 participants (35 women and 33 men) |
[26] |
|
Climate change |
Cook Islands, Niue, and New Zealand |
Mixed-methods (cross-sectional study) |
Consensus on key principles on mental health impacts from climate change |
|
|
70 expert panelists completed round 1 and (n = 58) round 2 (n = 59) |
[30] |
|
Climate change |
Bangladesh, Fiji, Vanuatu |
Qualitative method (cross-sectional study) |
Lived experiences and storylines related to well-being loss and healing in the context of climate change and violence against women and children (VAWC) |
Fiji
Vanuatu
|
|
Fiji
Vanuatu
|
[27] |
|
Climate change |
Australia, Cook Islands, Pacific Islands |
Mixed-methods (cross-sectional study) |
Expert perspectives on emotional responses and emerging mental and emotional aspects of environmental changes |
|
|
Pacific Islands 42 experts (stakeholders) Cook Islands 11 participants (4 women and 7 men) |
[31] |
|
Climate change |
Kiribati |
Mixed-methods (cross-sectional study) |
How people’s perceptions of both climate change impacts on water sources and their capacity to adapt to these impacts shape adaptation actions |
Perceptions of vulnerability and severity
|
|
132 participants |
[29] |
|
Climate change |
Kiribati |
Qualitative method (multi-year cross-sectional ethnographic study) |
Emotions and Christian religiosity and responses to climate change |
|
|
Not mentioned (since the methodological approach included listening to discourses, engaging in conversations, ethnographic interviews, and participant observation) |
[18] |
|
Climate change |
Tuvalu |
Mixed-methods (cross-sectional study) |
Idioms of distress, and determinants of distress |
|
|
16 key informants and 23 lay residents |
[32] |
|
Climate change |
Tuvalu |
Mixed methods (cross-sectional study) |
Psychological distress (culturally adapted version of the Hopkins-Symptom Checklist) and associated impairment due to local environmental impacts and abstract knowledge of climate change |
|
|
100 participants |
[20] |
|
Climate change |
Fiji |
Qualitative method (cross-sectional study) |
Observed environmental changes, adaptation efforts undertaken and challenges associated with activities, and the emotional experiences of villagers |
|
|
71 Indigenous Fijian adults (14 group interviews with 33 women and 38 men) |
[28] |
|
Climate change |
Fiji |
Mixed-methods (cross-sectional study) |
What people value, how climate change affects these values, and how to identify values-based ways of addressing loss and damage. |
|
|
27 participants (18 in depth interviews and two group interviews) |
[33] |
3.3. Factors Mediating the Relationships between Climate-Sensitive Hazard Exposure and Mental Health Impact
Factors mediating the relationship between climate-sensitive hazard exposures and mental health impacts are identified based on the conceptual framework of the social determinants of health [11] as shown in Figure 2. The pathways are based on our review, including disaster preparedness, other consequences, cultural factors, coping strategies, and barriers to mental healthcare, as summarized in Table S1. Underlying vulnerabilities, resilience, and preparedness may become evident after exposure, along with coping responses that directly affect socioeconomic status, environmental and livelihood, social structure and cultural values, physical health, and mental health. The impact on mental health could be exacerbated by emerging risks arising from interactions among these changes.
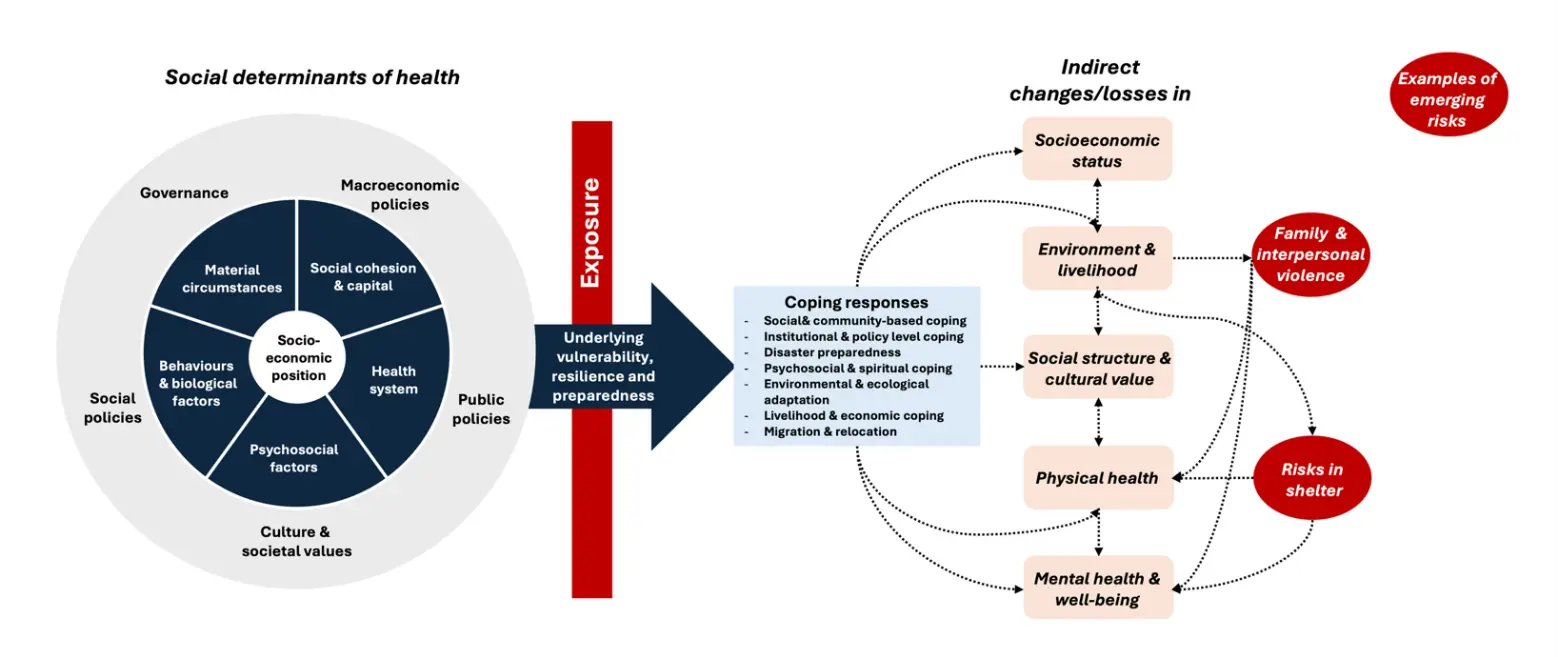
Figure 2. Factors mediating the relationships between climate-sensitive hazard exposures and mental health impacts.
3.3.1. Social Determinants of Health
Structural determinants and socioeconomic position, such as income, education, occupation, social class, gender, race, and ethnicity, are known to contribute to differential exposure and vulnerability to climate-sensitive hazards [11]. In our review, a few studies reported differential mental health impacts by socio-economic position. For example, occupational differences in risk perception of events were observed in the PICs, where farmers were primarily concerned about drought, whereas communal fishers were more affected by storms [19]. In addition, persons with disabilities, who often experience low socio-economic status in resource-limited settings, face heightened vulnerabilities during emergencies [22].
Intermediary determinants of health, such as material circumstances, psychosocial circumstances, behavioral and biological factors, and health systems, are influenced by socioeconomic position [11]. These determinants encompass underlying vulnerabilities, such as educational disparities [19] and infrastructure challenges in PICs. For example, inadequate irrigation systems in Fiji [24] and reliance on rainwater in Tuvalu increased vulnerability [22]. Community cohesion, reinforced by family networks [16,30,33] and social networks [17,23], strengthened the intra-island support system. Furthermore, PICs have strong community resilience [30], with community-led recovery efforts and collective participation in disaster response and societal rebuilding [27,30,32]. However, barriers to mental healthcare access can act as health system vulnerabilities during and after climate-sensitive hazard exposure. A shortage of mental health professionals and resources was identified, and fear of social stigma and gossip discourages individuals from discussing personal struggles, further limiting access to mental health support [32].
The impacts of climate-sensitive hazard exposure can differ by socioeconomic and political contexts, which consist of governance, macroeconomic policies, social policies, public policies, and cultural and societal values [11]. Disaster preparedness, which plays an important role during disasters, remains inadequate across PICs [20,31], with communities often relying on traditional knowledge for disaster response [22]. In Fiji, although climate change-related irrigation grant initiatives exist, they often fail to reach local communities [24]. In the Pacific context, social values, such as a strong connection to land, traditional knowledge [28], and cultural heritage [16] play a crucial role in shaping responses to environmental challenges. Religion also serves as a significant influence, with spiritual faith providing support in Samoa [16], and faith in God reported across multiple PICs, including the Cook Islands, Kiribati, and Tuvalu [18,22,23,29,32]. In addition, culturally, many PICs prefer traditional healing methods over clinical treatment [30].
3.3.2. Coping Response
PICs implemented or proposed a broad range of coping strategies in response to climate-sensitive hazard exposures. Social and community-based coping, such as kinship ties [23], traditional support systems [15], churches, schools, and cultural education, play a critical role in fostering emotional resilience [21]. The involvement of persons with disabilities in decision-making [22] and the support of trusted family networks further strengthen communal coping capacities [24]. Institutional and policy-level strategies include government-led efforts like Fiji’s tuition-free education policy [24], climate change awareness campaigns [18], capacity-building programs [30], and locally tailored climate change adaptation planning [17]. Disaster preparedness that includes early warning systems [24], land-use planning [19], and water storage infrastructure needs to be improved [29]. Psychosocial and spiritual coping, including prayer [32], traditional healing practices [15], and sharing of traumatic stories, could provide culturally grounded support. Efforts to restore the socio-ecological systems and protect cultural knowledge and sacred places underscore the role of cultural continuity in resilience [33]. Livelihood strategies such as livelihood diversification, engagement in new markets [24], and planting drought-tolerant crops may support economic recovery [27], although vulnerable groups, particularly women and children, may be forced to sell their products on the streets [27]. Finally, migration and planned relocation, including resettlement to higher ground or to other countries like New Zealand, also serve as long-term adaptation strategies [16,18,26,28,29].
3.3.3. Indirect Impacts on Mental Health through Emerging Risks
Environmental and livelihood disruptions are consequences of extreme events. Sea level rise led to the inundation of villages, limited space to build houses, and contamination of taro pits, forcing some people to relocate their homes [25,29]. These changes were reported to affect daily life and contribute to worry about the future [25,29]. Similarly, tropical cyclones caused coastal areas to be washed away and made it difficult for affected communities to return to normal life [23,31]. Droughts reduced farmers’ household income and increased the risk of food insecurity [24]. Cyclones disrupted marketplace operations, particularly affecting women, making them feel dependent on men and resulting in a loss of well-being, as they were unable to support their households [27]. In addition, climate change-driven cultural changes may undermine values that traditionally protected families during financial hardship by shifting traditional subsistence livelihoods toward monetary income and increasing dependence on imported food [32]. Food and water insecurity is another major concern, as droughts [19,23,24] and sea level rise [25] reduced access to safe water and agricultural productivity, leading to famine, malnutrition, and the need for humanitarian aid [19]. The planned relocation also led to notable changes in lifestyle and social behavior. Reports indicate increased consumption of packaged goods and alcohol, reflecting shifts in dietary patterns among some residents, which may act as risk amplifiers of broader health threats [17].
Extreme events have been shown to cause profound socio-cultural losses. Several studies reported that the loss of culture and connection to ancestors and history disrupted identity and traditions [23,28,30]. Migration, displacement, and planned relocation weakened social structures and traditional values [30]. In addition to these disruptions, affected populations experienced the loss of family members, as well as plants and animals, which further contributed to grief and emotional distress [15,16,26]. Furthermore, the inability to carry out traditional funeral practices due to inadequate post-disaster conditions intensified emotional and cultural distress [16].
Emerging risks often arise during and after extreme events. Inadequate shelter conditions pose significant challenges. For example, overcrowded evacuation centers in Fiji were reported to lack privacy, potentially threatening privacy, safety, and reproductive health, particularly for pregnant women and individuals during their menstruation period, who may receive inappropriate care [27]. Climate change also tends to exacerbate pre-existing gender inequalities. In many cases, the burden of household responsibilities increases for women, and conditions of violence and domestic abuse have been observed to worsen during and after extreme events [27]. Planned relocation may also unintentionally heighten family violence. In some cases, the shift from communal living to individual housing has provided more private space, which has been associated with increased incidents of family violence.
4. Discussion
In this scoping review, we identified 19 studies that reported on climate change and mental health outcomes in PICs. Our review had three key findings. First, both acute and slow-onset events were associated with a wide range of adverse mental health outcomes, including distress, anxiety, depression, and ecological grief. However, only one study employed quantitative methods, highlighting a gap in measuring the prevalence of mental distress. Second, the relationship between climate-sensitive hazard exposures and mental health was shaped by multiple social determinants of health, including structural determinants and socioeconomic position, intermediary determinants of health, and broader socioeconomic and political context. While community cohesion and traditional support systems often contributed to resilience during disasters, limited preparedness, stigma, and lack of access to mental health services increased vulnerability. Third, climate-related events and associated coping mechanisms frequently resulted in indirect consequences that generated new risks, such as gender-based violence and risks in shelter conditions. In this section, we discuss each key finding in detail and conclude with recommendations for further study and action.
The first key finding highlights the diverse and multifaceted mental health impacts of climate change in PICs, consistent with global patterns, while emphasizing unique contextual factors. Our study found similar results to a global review that reported a high prevalence of depression, anxiety, suicide, non-specific psychological distress, worry, grief, and frustration associated with slow-onset climate stressors [34]. However, the number and scope of quantitative research studies from low-resource settings on climate-related mental health impacts remain limited, mirroring the regional research gaps noted in North America, where studies were mostly conducted in the United States and Canada, with only a few from Mexico [35]. Importantly, our findings underscore the significance of context-specific definitions of health in shaping mental health outcomes. For example, in Samoa, health is conceptualized not only in biomedical terms but also through spiritual, physical, mental, and other social dimensions, with culture and family playing key roles [36]. Although our review could not identify the protective factors within the included studies, previous research documented the role of community cohesion as a buffer following acute events such as hurricanes and floods, highlighting the importance of social connectedness in supporting mental health and resilience [35]. In Bangladesh, some individuals displaced after landslides experienced improved mental well-being through increased economic stability, optimism, safety, and community closeness [37].
Our second key finding underscores that the relationship between climate-sensitive hazard exposure and mental health is deeply shaped by multiple social determinants of health. Climate change acts as a risk amplifier, disrupting the foundational conditions that support mental health, such as stable housing, employment, cultural and environmental conditions, and living and working conditions [3]. Vulnerable populations, particularly those with limited access to resources, information, and protection, experience intensified mental health challenges as a result [38]. Among Pacific Islanders, including the Indigenous population, cultural values further mediate this relationship [7]. For many, land is a vital source of life, connecting people to their past, present, and future [7]. This deep cultural attachment increases psychological vulnerability. When extreme events disrupt land access or alter ecosystems, the resulting distress can be profound. Similarly, Inuit populations on the frontlines of climate change face profound disruptions to their livelihoods and identities, compounded by pre-existing health disparities and precarious living conditions [39]. These disruptions contribute to emotional distress, including grief over the loss of land-based practices, increased family stress, substance use, and a potential rise in suicidal ideation [39].
The third key finding from this study is that communities across PICs have developed diverse coping responses to extreme events. Coping involves on immediate responses to constraints and survival, and communities are resilient when past adaptation efforts align their coping range with the hazards they regularly encounter [40]. In PICs, traditional coping strategies were used in response to disasters and climate change, including traditional practices, faith, local governance and leadership, community support, and food security [41]. Furthermore, mental health and psychological support could be implemented at multiple levels, including individuals, groups, local media and institutions, and larger social structures, through diverse mechanisms such as psychotherapy, resilience-building programs, nature-based activities, and strengthening community networks [42]. In Samoa, post-disaster care included culturally embedded partnerships among Samoan therapists, Samoan catholic pastoral workers, and non-Samoan clinicians, who together conducted household visits to tsunami-affected families [43]. Similarly, in the Solomon Islands, community members typically seek help first from traditional healers and churches, turning to Western medicine only as a last resort [44]. Despite the availability of some mental healthcare services, significant barriers to care remain, including stigma and reluctance to discuss personal emotions, even within families [39]. Moreover, services perceived as "Western" are often mistrusted or viewed as culturally inappropriate due to a lack of contextual adaptation [40].
We also identified multiple and compounding disasters, as well as emerging risks that mediate through changes and losses in socioeconomic status, the environment and livelihoods, cultural values, physical and mental health, and coping strategies. The challenges of multiple and compounding disasters further complicate the pace of response and recovery. Repeated exposure to extreme events can strain healthcare facilities, alter public risk perception, and weaken governmental capacity for response [45]. Currently, in low-resource settings, recovery efforts have included food security initiatives, microcredit programs, global water, sanitation, and hygiene (WASH) programs, and recovery aid programs [45], but these programs often fail to reflect the realities of a consecutive disaster context. Coping capacity depends on available resources, but repeated reliance on coping without recovery can deplete these resources and increase long-term vulnerability to future hazards [40]. Therefore, current risk management efforts are not keeping pace with rising climate threats, limiting opportunities for timely and effective response [46]. For example, in Vanuatu, which experienced consecutive cyclones in 2023, residents reported that life remained difficult a year later, illustrating the lack of recovery time following repeated disasters [46]. Furthermore, beyond immediate impacts, climate change contributes to cascading and emergent risks across ecological and social systems. Rising temperatures and extreme weather amplify existing stressors and inequities, disproportionately affecting individuals with fewer economic resources, pre-existing mental health conditions, or higher exposure to extreme events [3,47]. These interconnected systems generate compounding, cascading, and aggregate risks arising from interactions among various determinants of risk [48].
4.1. Additional Knowledge Gaps
In addition to the key findings, this review identified several important knowledge gaps. First, there is limited baseline knowledge on the prevalence and burden of mental health conditions in PICs, which makes it difficult to assess changes over time or determine the relative impact of climate-related events. While some studies employed tools such as the Impact of Event Scale-Revised (IES-R) and the Hopkins Symptom Checklist-25 (HSCL-25), quantitative data that integrates cultural context remains scarce. Therefore, culturally adapted survey instruments are needed better to understand mental health outcomes in the Pacific context. Second, there was a lack of understanding of the cumulative mental health impacts of multiple and sequential disaster events, such as cyclones, droughts, and sea-level rise, that occur over time. Because PICs experience both slow-onset and acute events, cumulative impacts and community capacity for recovery need to be considered when assessing mental health impacts. Third, although cultural factors such as religion, traditional healing practices, and community-based support are often mentioned, there is insufficient integration of these elements into formal mental health adaptation strategies. Future research should center on culturally grounded frameworks to co-develop effective, equitable, and context-specific interventions. For example, tools such as stress testing and a desk-based scenario exercise could help anticipate and prepare for conditions beyond historical precedent and build proactive, cost-effective risk management strategies by promoting cross-sectoral collaboration and resilience [49]. For instance, a stress-testing scenario in a coastal regional capital of a low-income country in November 2046 simulates a tropical cyclone striking during a prolonged drought, challenging hospital surge capacity and the emergency response system, and highlighting the need for multisectoral coordination [50]. By envisioning outcomes as realistically as possible, such exercises enable organizations to identify opportunities for strengthening climate-resilient health systems in a changing climate [50].
4.2. Limitations
Several limitations should be considered when interpreting the findings of this review. First, we included only literature published in English, which may have led to the exclusion of valuable research conducted in other languages in PICs. This would reinforce the structural dominance of English-language science and may not fully reflect the mental health impacts in Pacific contexts. Second, although the search strategy employed a wide range of synonyms for climate-sensitive hazards, the outcome search relied primarily on the MeSH term “mental health”. This may have excluded studies that focused on specific conditions such as anxiety, depression, post-traumatic stress disorder (PTSD), or grief, thereby narrowing the scope of retrieved evidence. Third, the variation in study designs and the predominance of qualitative and mixed-methods approaches limited our ability to synthesize findings quantitatively. Fourth, most studies focused on a single climate-related exposure and utilized cross-sectional designs, with limited consideration of multiple or compounding events and a wide range of timeframes for assessing mental health outcomes. Fifth, title, abstract, and full-text screening were conducted by a single reviewer, which introduces potential bias. Similarly, data extraction was also performed by a single individual, further increasing the possibility of subjectivity or error. Finally, because scoping reviews aim to map the breadth of available evidence rather than assess study quality, a critical appraisal of included studies was not conducted. While consistent with scoping review methodology, this limits the robustness of the assessment.
5. Conclusions
This scoping review examined how climate change affects mental health in PICs, revealing that both acute and slow-onset extreme events are linked to adverse mental health outcomes, including distress, anxiety, depression, and ecological grief. Our findings highlight the critical role of social determinants and cultural context in shaping vulnerability and resilience in PICs. However, notable gaps persist, including limited quantitative data, a lack of standardized and culturally adapted measurement tools, and scarce research on the cumulative effects of multiple climate change-related disasters, as well as emerging risks arising from changes and coping strategies. Additionally, culturally embedded coping strategies and traditional healing practices play important roles and should be integrated into the mental health adaptation plans to ensure culturally and contextually appropriate responses.
Supplementary Materials
The following supporting information can be found at: https://www.sciepublish.com/article/pii/745, Table S1: Detailed summary of key results from included articles.
Author Contributions
Conceptualization, H.P., J.J.H. and K.L.E.; Literature review, H.P.; Writing—Original Draft Preparation, H.P.; Writing—Review & Editing, H.P., J.J.H. and K.L.E.; Visualization, H.P.; Supervision, J.J.H. and K.L.E.; Funding Acquisition, J.J.H. and K.L.E.
Ethics Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
This is a scoping review article based on findings in published literature and did not involve analysis of newly generated data.
Funding
This research was funded by New Frontiers in Research Fund-International (NFRF-I Climate Mental Health Research Initiative), grant number NFRFI-2023-00240.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
-
Kim H, Ryan A, Harding AB, Moskowitz AF, Passe AI, Kawazu EC. Health risks of climate change in the 21 Pacific Island states and noted gaps in scientific evidence: A scoping review. J. Clim. Change Health 2022, 8, 100166. doi:10.1016/j.joclim.2022.100166. [Google Scholar]
-
Pörtner HO, Roberts DC, Poloczanska ES, Mintenbeck K, Tignor M, Alegría A, et al. (Eds.) Summary for Policymakers. In Climate Change 2022—Impacts, Adaptation and Vulnerability: Working Group II Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2023; pp. 3–33. [Google Scholar]
-
Lawrance EL, Thompson R, Newberry Le Vay J, Page L, Jennings N. The Impact of Climate Change on Mental Health and Emotional Well-being: A Narrative Review of Current Evidence, and its Implications. Int. Rev. Psychiatry 2022, 34, 443–498. doi:10.1080/09540261.2022.2128725. [Google Scholar]
-
Huang W, Gao Y, Xu R, Yang Z, Yu P, Ye T, et al. Health Effects of Cyclones: A Systematic Review and Meta-Analysis of Epidemiological Studies. Environ. Health Perspect. 2023, 131, 86001. doi:10.1289/EHP12158. [Google Scholar]
-
Tasdik Hasan M, Adhikary G, Mahmood S, Papri N, Shihab HM, Kasujja R, et al. Exploring mental health needs and services among affected population in a cyclone affected area in costal Bangladesh: A qualitative case study. Int. J. Ment. Health Syst. 2020, 14, 12. doi:10.1186/s13033-020-00351-0. [Google Scholar]
-
Zhao H, He L, Liu C, Shan XB, Gui CY, Zhang L, et al. Self-harm and interpersonal violence due to high temperature from the global burden of disease study 2019: A 30-year assessment. Environ. Res. 2024, 243, 117826. doi:10.1016/j.envres.2023.117826. [Google Scholar]
-
Dickie R, Maly KE. Indigenous Traditions and Sacred Ecology in the Pacific Islands. UW-L J. Undergrad. Res. 2005, 8, 1–9. [Google Scholar]
-
Cutrer-Párraga EA, Allen GEK, Miller EE, Garrett MF, Conklin H, Franklin CN, et al. Perceptions and Barriers About Mental Health Services Among Pacific Islanders: An Interpretative Phenomenological Analysis. J. Couns. Psychol. 2024, 71, 89–103. doi:10.1037/cou0000719. [Google Scholar]
-
Charlson FJ, Diminic S, Whiteford HA. The Rising Tide of Mental Disorders in the Pacific Region: Forecasts of Disease Burden and Service Requirements from 2010 to 2050. Asia Pac. Policy Stud. 2015, 2, 280–292. doi:10.1002/app5.93. [Google Scholar]
-
Mengesha NA, Sarnyai Z. The mental health impact of climate change on Pacific Islanders: A systematic review focused on sea level rise and extreme weather events. Australas. Psychiatry 2025, 33, 220–227. doi:10.1177/10398562241312865. [Google Scholar]
-
WHO Social Determinants of Health. A Conceptual Framework for Action on the Social Determinants of Health; WHO: Geneva, Switzerland, 2010. [Google Scholar]
-
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. doi:10.1186/s12874-018-0611-x. [Google Scholar]
-
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. doi:10.7326/m18-0850. [Google Scholar]
-
Bernard N, Sagawa Y, Jr., Bier N, Lihoreau T, Pazart L, Tannou T. Using artificial intelligence for systematic review: The example of elicit. BMC Med. Res. Methodol. 2025, 25, 75. doi:10.1186/s12874-025-02528-y. [Google Scholar]
-
Pomer A, Buffa G, Ayoub MB, Taleo F, Sizemore JH, Tokon A, et al. Psychosocial distress among women following a natural disaster in a low- to middle-income country: "healthy mothers, healthy communities" study in Vanuatu. Arch. Women Ment. Health 2019, 22, 825–829. doi:10.1007/s00737-019-00980-6. [Google Scholar]
-
Seiuli BMS, Nikora LW, Awekotuku NT, Hodgetts D. Fia Ola: Grief Recovery Following a Tsunami Disaster in Samoa. J. Pac. Rim Psychol. 2016, 10, e5. doi:10.1017/prp.2016.2. [Google Scholar]
-
McMichael C, Powell T. Planned Relocation and Health: A Case Study from Fiji. Int. J. Environ. Res. Public Health 2021, 18, 4355. doi:ARTN 4355 10.3390/ijerph18084355. [Google Scholar]
-
Hermann E. Climate Change, Emotions and Religion: Imagining the Future in Central Oceania. Anthr. Forum 2020, 30, 274–291. doi:10.1080/00664677.2020.1812051. [Google Scholar]
-
Lohmann P, Pondorfer A, Rehdanz K. Natural Hazards and Well-Being in a Small-Scale Island Society. Ecol. Econ. 2019, 159, 344–353. doi:10.1016/j.ecolecon.2018.12.023. [Google Scholar]
-
Gibson KE, Barnett J, Haslam N, Kaplan I. The mental health impacts of climate change: Findings from a Pacific Island atoll nation. J. Anxiety Disord. 2020, 73, 102237. doi:10.1016/j.janxdis.2020.102237. [Google Scholar]
-
Crookes AE, Warren MA, Meyer S. When threat is imminent, does character matter for climate action? Exploring environmental concerns, well-being, and character strengths in the Pacific Island Countries. S. Afr. J. Psychol. 2022, 52, 436–448. doi:10.1177/00812463221129361. [Google Scholar]
-
Elisala N, Turagabeci A, Mohammadnezhad M, Mangum T. Exploring persons with disabilities preparedness, perceptions and experiences of disasters in Tuvalu. PLoS ONE 2020, 15, e0241180. doi:10.1371/journal.pone.0241180. [Google Scholar]
-
Clissold R, McNamara KE, Westoby R, Wichman V. Experiencing and responding to extreme weather: Lessons from the Cook Islands. Local Environ. 2023, 28, 645–661. doi:10.1080/13549839.2023.2169912. [Google Scholar]
-
Nand MM, Bardsley DK, Suh J. Climate change loss and damage from droughts: Key insights from Fiji's sugar industry. Local Environ. 2025, 30, 778–794. doi:10.1080/13549839.2024.2386963. [Google Scholar]
-
Asugeni J, MacLaren D, Massey PD, Speare R. Mental health issues from rising sea level in a remote coastal region of the Solomon Islands: Current and future. Australas. Psychiatry 2015, 23, 22–25. doi:10.1177/1039856215609767. [Google Scholar]
-
du Bray M, Wutich A, Larson KL, White DD, Brewis A. Anger and Sadness: Gendered Emotional Responses to Climate Threats in Four Island Nations. Cross-Cult. Res. 2019, 53, 58–86. doi:10.1177/1069397118759252. [Google Scholar]
-
Ayeb-Karlsson S, Chandra A, McNamara KE. Stories of loss and healing: Connecting non-economic loss and damage, gender-based violence and well-being erosion in the Asia-Pacific region. Clim. Change 2023, 176, 157. doi:10.1007/s10584-023-03624-y. [Google Scholar]
-
Lykins AD, Cosh S, Nunn PD, Kumar R, Sundaraja C. “Io, Keimami Leqataka Vakalevu Na Vei Gauna Mai Muri” (“We are Worried About the Future Generation”): Experiences of Eco-Grief in Rural Indigenous Fijians. Glob. Environ. Psychol. 2023, 1, 1–28. doi:10.5964/gep.11447. [Google Scholar]
-
Kuruppu N, Liverman D. Mental preparation for climate adaptation: The role of cognition and culture in enhancing adaptive capacity of water management in Kiribati. Glob. Environ. Change 2011, 21, 657–669. doi:10.1016/j.gloenvcha.2010.12.002. [Google Scholar]
-
Tiatia J, Langridge F, Newport C, Underhill-Sem Y, Woodward A. Climate change, mental health and well-being: Privileging Pacific peoples’ perspectives—Phase one. Clim. Dev. 2023, 15, 655–666. doi:10.1080/17565529.2022.2145171. [Google Scholar]
-
Clissold R, McNamara KE, Westoby R. Emotions of the Anthropocene across Oceania. Int. J. Environ. Res. Public Health 2022, 19, 6757. doi:10.3390/ijerph19116757. [Google Scholar]
-
Gibson K, Haslam N, Kaplan I. Distressing encounters in the context of climate change: Idioms of distress, determinants, and responses to distress in Tuvalu. Transcult. Psychiatry 2019, 56, 667–696. doi:10.1177/1363461519847057. [Google Scholar]
-
Nand MM, Clissold R, McNamara KE, Yee M. Guiding our responses to climate change by what people value: Insights from Fiji. Geoforum 2024, 155, 104080. doi:10.1016/j.geoforum.2024.104080. [Google Scholar]
-
Burrows K, Denckla CA, Hahn J, Schiff JE, Okuzono SS, Randriamady H, et al. A systematic review of the effects of chronic, slow-onset climate change on mental health. Nat. Ment. Health 2024, 2, 228–243. doi:10.1038/s44220-023-00170-5. [Google Scholar]
-
Aylward B, Ashlee C, Rachael V, Harper SL. Climate change is impacting mental health in North America: A systematic scoping review of the hazards, exposures, vulnerabilities, risks and responses. Int. Rev. Psychiatr. 2022, 34, 34–50. doi:10.1080/09540261.2022.2029368. [Google Scholar]
-
Goodyear-Smith F, 'Ofanoa M. Fa'afaletui: A Pacific Research Framework. J. Mix. Method. Res. 2022, 16, 34–46. doi:10.1177/1558689820985948. [Google Scholar]
-
Burrows K, Pelupessy DC, Khoshnood K, Bell ML. Environmental Displacement and Mental Well-Being in Banjarnegara, Indonesia. Environ. Health Perspect. 2021, 129, 117002. doi:10.1289/EHP9391. [Google Scholar]
-
Cianconi P, Betro S, Janiri L. The Impact of Climate Change on Mental Health: A Systematic Descriptive Review. Front. Psychiatry 2020, 11, 74. doi:10.3389/fpsyt.2020.00074. [Google Scholar]
-
Bourque F, Willox AC. Climate change: The next challenge for public mental health? Int. Rev. Psychiatry 2014, 26, 415–422. doi:10.3109/09540261.2014.925851. [Google Scholar]
-
Seneviratne SI, Nicholls N, Easterling D, Goodess CM, Kanae S, Kossin J, et al. 2012: Changes in climate extremes and their impacts on the natural physical environment. In Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation; Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, Eds.; A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change (IPCC); Cambridge University Press: Cambridge, UK; New York, NY, USA, 2012; pp. 109–230. [Google Scholar]
-
Fletcher SM, Thiessen J, Gero A, Rumsey M, Kuruppu N, Willetts J. Traditional coping strategies and disaster response: Examples from the South Pacific region. J. Environ. Public Health 2013, 2013, 264503. doi:10.1155/2013/264503. [Google Scholar]
-
Xue S, Massazza A, Akhter-Khan SC, Wray B, Husain MI, Lawrance EL. Mental health and psychosocial interventions in the context of climate change: A scoping review. NPJ Ment. Health Res. 2024, 3, 10. doi:10.1038/s44184-024-00054-1. [Google Scholar]
-
Tamasese TK, Parsons TL, Waldegrave C, Sawrey R, Bush A. Asiasiga: A Samoan intervention to address the immediate mental health needs of Samoan communities after a tsunami. Australas. Psychiatry 2020, 28, 31–33. doi:10.1177/1039856219866321. [Google Scholar]
-
MacLaren D, Asugeni J, Asugeni R, Kekeubata E. Incorporating sociocultural beliefs in mental health services in Kwaio, Solomon Islands. Australas. Psychiatry 2009, 17 (Suppl. S1), S125–S127. doi:10.1080/10398560902948381. [Google Scholar]
-
Leppold C, Gibbs L, Block K, Reifels L, Quinn P. Public health implications of multiple disaster exposures. Lancet Public Health 2022, 7, e274–e286. doi:10.1016/S2468-2667(21)00255-3. [Google Scholar]
-
Ebi KL. Understanding the risks of compound climate events and cascading risks. Dialogues Clim. Change 2025, 2, 33–37. doi:10.1177/29768659241304857. [Google Scholar]
-
Heinz A, Brandt L. Climate change and mental health: Direct, indirect, and intersectional effects. Lancet Reg. Health-Eur. 2024, 43, 100969. doi:10.1016/j.lanepe.2024.100969. [Google Scholar]
-
Simpson NP, Mach KJ, Constable A, Hess J, Hogarth R, Howden M, et al. A framework for complex climate change risk assessment. One Earth 2021, 4, 489–501. doi:10.1016/j.oneear.2021.03.005. [Google Scholar]
-
Ebi KL, Berry P, Hayes K, Boyer C, Sellers S, Enright PM, et al. Stress Testing the Capacity of Health Systems to Manage Climate Change-Related Shocks and Stresses. Int. J. Environ. Res. Public Health 2018, 15, 2370. [Google Scholar]
-
Berry P, Ebi KL, Enright P. Chapter 20: Developing health system resilience for the climate crisis. In Handbook of Health System Resilience; Edward Elgar Publishing: Cheltenham, UK, 2024; pp. 307–328. [Google Scholar]